Polymyalgia Rheumatica vs Fibromyalgia: Similarities & Differences
September 2, 2025

- Overlap in symptoms: Both polymyalgia rheumatica (PMR) and fibromyalgia can involve widespread pain, stiffness, and fatigue, which often makes them difficult to tell apart.
- Underlying causes differ: PMR is an inflammatory condition affecting adults over 50, while fibromyalgia is linked to changes in how the nervous system processes pain and can affect people at any age.
- Diagnosis matters: Only a doctor can confirm which condition is present. Blood tests and imaging often point to PMR, while fibromyalgia is identified after ruling out other causes.
- Management approaches: Each condition is addressed differently under medical care. Tracking symptoms, sleep, and treatments with tools like Human Health can support better day-to-day management and more informed conversations with healthcare providers.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is for educational purposes only and is not a substitute for professional medical care. Always speak with a qualified healthcare provider about any questions you may have regarding a medical condition.
When persistent pain and fatigue disrupt your daily life, it’s natural to wonder what’s really going on. Two conditions often compared are polymyalgia rheumatica (PMR) and fibromyalgia. Both can cause widespread aches and stiffness, but they stem from very different processes.
PMR is an inflammatory condition that mostly affects people over 50, while fibromyalgia is linked to heightened sensitivity in the nervous system and can appear at any age.
In this article, we’ll break down the key similarities and differences between the two, explain how doctors distinguish them, and show how symptom tracking can support clearer conversations with your healthcare provider.
What is polymyalgia rheumatica (PMR)?
Polymyalgia rheumatica is an inflammatory condition that mainly affects adults over the age of 50. It causes stiffness, aching, and reduced movement in large muscle groups, particularly around the shoulders, hips, and neck. Symptoms are often worse in the morning or after long periods of rest.
Doctors typically use blood tests and imaging to check for signs of inflammation when investigating PMR. Because these symptoms can overlap with other conditions, only a healthcare provider can confirm the diagnosis.
What is fibromyalgia?
Fibromyalgia is a chronic condition where the nervous system becomes more sensitive to pain signals. This heightened sensitivity can lead to widespread pain, fatigue, sleep problems, and difficulties with concentration, often referred to as “fibro fog.” Unlike polymyalgia rheumatica (PMR), fibromyalgia does not show up in standard blood tests or imaging, which makes diagnosis more challenging.
Because its symptoms overlap with many other conditions, doctors usually identify fibromyalgia by excluding other causes. Keeping a consistent record of symptoms such as pain intensity, sleep quality, and fatigue can help provide useful context during medical evaluations.
Similarities between polymyalgia rheumatica and fibromyalgia
PMR and fibromyalgia are distinct conditions, but they overlap in several ways that can make them difficult to tell apart without medical evaluation.

Widespread pain
Both conditions cause pain across large muscle groups, often affecting the shoulders, hips, and back. This discomfort can feel similar day to day, which is why many people confuse the two. In PMR, the pain is linked to inflammation, whereas in fibromyalgia it stems from nervous system sensitivity.
Morning stiffness and fatigue
People with PMR and fibromyalgia often struggle with stiffness after waking and feel fatigued even after rest. This overlap can make mornings particularly difficult. A key distinction is that PMR stiffness typically eases with movement, while fibromyalgia fatigue and muscle soreness may persist throughout the day.
Sleep difficulties
Disrupted sleep is common in both conditions, and poor rest can worsen pain and fatigue. Fibromyalgia often involves non-restorative sleep and “fibro fog,” while PMR sleep problems usually result from pain and stiffness, making it hard to stay comfortable at night.
Impact on daily life
Both conditions can limit mobility, reduce energy, and interfere with work, hobbies, or social activities. The day-to-day impact looks similar on the surface, but PMR is usually more sudden in onset, while fibromyalgia tends to develop gradually and fluctuate in intensity over time.
Need for medical evaluation
Neither condition can be self-diagnosed. Because they share pain, stiffness, and fatigue, only a doctor can sort them apart. Blood tests and imaging often show inflammation in PMR, whereas fibromyalgia is usually identified after other possible causes have been ruled out.
Key differences between polymyalgia rheumatica and fibromyalgia
While PMR and fibromyalgia share some symptoms, the underlying causes and diagnostic approaches are very different.
Age group
- PMR: Almost always affects people over the age of 50, with the highest risk between 70 and 80.
- Fibromyalgia: Can appear at any age, including young adults and even teenagers, but is more often diagnosed in women.
- Key distinction: Age alone does not confirm a diagnosis, but if you are under 50, fibromyalgia is far more likely than PMR.
Underlying biology
- PMR: Driven by inflammation in muscles and connective tissues, especially around large joints like the shoulders and hips.
- Fibromyalgia: Involves changes in how the nervous system processes pain signals, leading to heightened sensitivity.
- Key distinction: PMR has measurable inflammation, while fibromyalgia does not show inflammation in tests. This biological difference is central to diagnosis.
Diagnostic approach
- PMR: Blood tests often show elevated markers of inflammation, such as ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein). Imaging may confirm inflammation.
- Fibromyalgia: No lab or imaging test exists. Doctors diagnose it by excluding other conditions and assessing symptom history.
- Key distinction: If inflammation shows clearly on tests, PMR is more likely. Fibromyalgia remains a diagnosis of exclusion.
Symptom patterns
- PMR: Stiffness and aching are concentrated in the shoulders, hips, and neck. Morning symptoms are usually the worst and may ease with movement.
- Fibromyalgia: Pain is widespread across the body and often comes with fatigue, sleep disturbances, and cognitive difficulties (“fibro fog”).
- Key distinction: PMR pain is localized and inflammation-driven, while fibromyalgia symptoms are more widespread and include neurological aspects beyond pain.
How do I know which one I have?
Because polymyalgia rheumatica and fibromyalgia can look similar, the only way to know for sure is through medical evaluation. PMR is more likely if you are over 50 and experiencing sudden stiffness in the shoulders and hips, while fibromyalgia can affect people at any age and usually comes with fatigue, sleep problems, and cognitive symptoms.
Doctors may use blood tests or imaging to look for inflammation when investigating PMR. With fibromyalgia, diagnosis usually involves ruling out other conditions.
Keeping a detailed record of your symptoms, including when they appear, how long they last, and what makes them better or worse, can give your healthcare provider valuable insights and help them reach a clearer conclusion.
{{inline-cta-1}}
Can I have both polymyalgia rheumatica and fibromyalgia?
It is possible for someone to be diagnosed with both conditions, though it is not very common. Because PMR and fibromyalgia involve different biological processes, they can overlap in the same person, making it harder to distinguish which symptoms belong to which condition. This is why tracking patterns over time and sharing them with your healthcare provider can be so valuable.
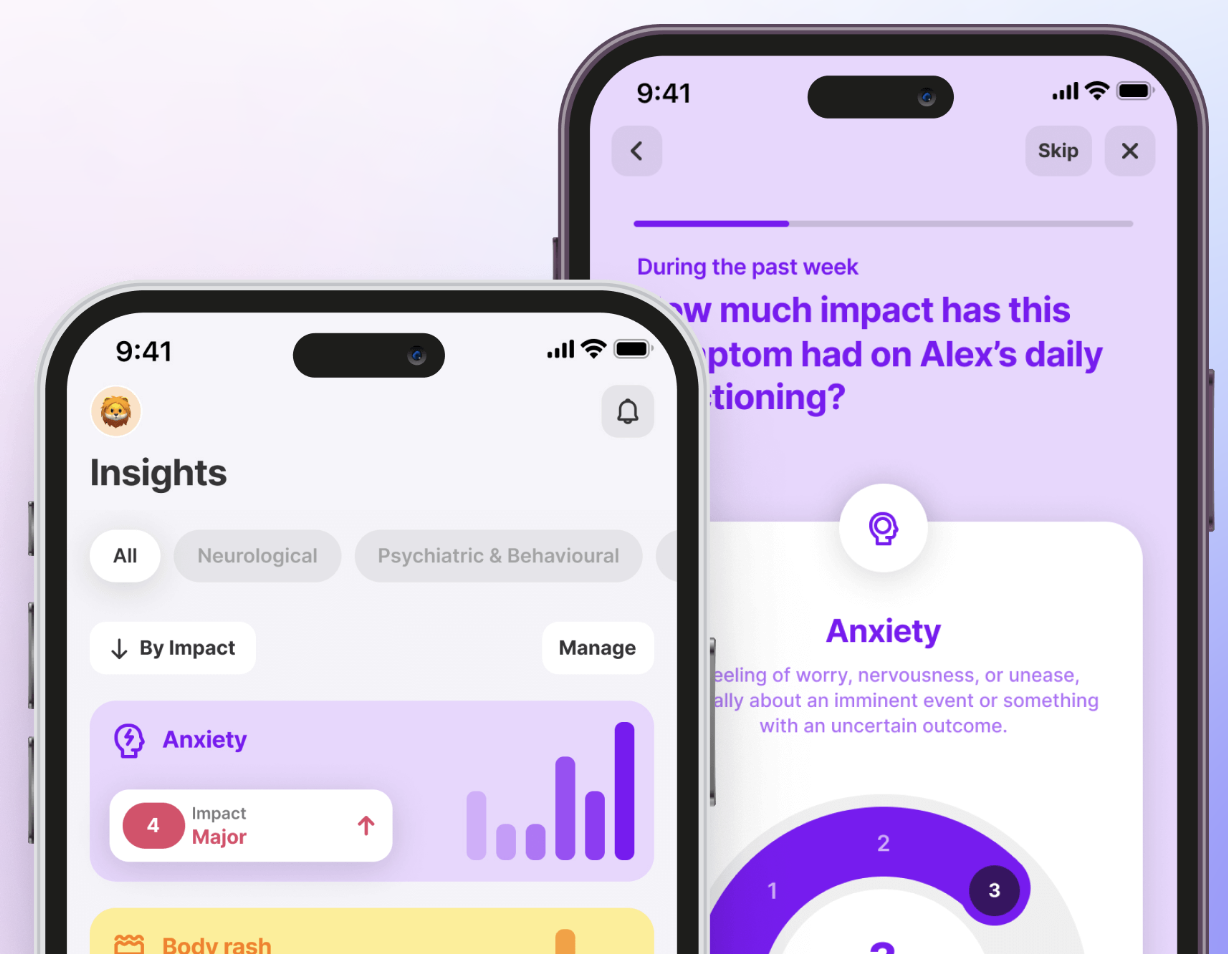
Using the Human Health app, you can log daily pain levels, stiffness, fatigue, and sleep quality. These records can then be exported as a summary to support clearer conversations with your doctor about whether symptoms may point to one condition, both, or something else.
Treatments & management for polymyalgia rheumatica and fibromyalgia
While both conditions involve chronic pain and fatigue, their management approaches are different and must be guided by a healthcare provider. Tracking symptoms and responses to lifestyle changes can play an important role in both cases.
Polymyalgia rheumatica (PMR)
PMR is usually addressed through medical care that targets inflammation, under a doctor’s supervision. Lifestyle strategies such as gentle movement, stretching, and consistent sleep routines may also help some people cope day to day. Because treatment often includes medications, tracking them can be an important part of managing care.
The Human Health app offers a medication tracker that lets you log doses, side effects, and adherence. This record makes it easier to spot patterns and share accurate updates with your healthcare provider during appointments.

Fibromyalgia
Management for fibromyalgia often involves a combination of approaches, including exercise, sleep support, and stress reduction. Some people also explore therapies like mindfulness, gentle yoga, or pacing techniques to balance energy levels. Since fibromyalgia symptoms can shift daily, logging fatigue, sleep quality, and pain intensity helps individuals and their healthcare providers identify what makes symptoms better or worse.
Track & understand your symptoms better with the Human Health app
Living with unexplained pain or fatigue can be confusing, especially when symptoms overlap between conditions like PMR and fibromyalgia. While only a healthcare provider can confirm a diagnosis, you can take an active role by tracking your daily experiences.
The Human Health app makes this easier. You can log pain levels, stiffness, sleep, and energy, then export a summary to share with your doctor. These insights not only support better conversations but also help you spot your own patterns over time.
Start tracking today and take the first step toward clearer answers and more informed care.
Sources:
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Take Control of Your Health With The Human Health App
Living with a chronic condition can be complex. The Human Health app helps you track your health, find what truly works, and get the support you need - on your own or alongside your care team.








.jpg)





.png)

