Fibromyalgia vs. MS: Symptoms, Causes, and How to Tell the Difference
October 2, 2025

- Fibromyalgia and multiple sclerosis (MS) are two distinct conditions - fibromyalgia is a chronic pain syndrome, while MS is an autoimmune disease that damages the nervous system.
- Key differences include cause and progression: fibromyalgia has no known structural damage, whereas MS involves immune-driven nerve damage seen on scans.
- Symptoms can overlap, such as fatigue, brain fog, and widespread pain, making diagnosis challenging.
- Accurate diagnosis and management require medical evaluation, but using tools like the Human Health app’s symptom tracker can help you log patterns and share them with your healthcare provider for better clarity.
Disclaimer: This article is for informational and educational purposes only. It is not medical advice, and it should not be used to diagnose, treat, cure, or prevent any condition. Always talk with a qualified healthcare provider about your health concerns before making decisions about diagnosis, treatments, or medications.
Living with unexplained fatigue, pain, or brain fog can be confusing and frustrating. It is natural to wonder what is causing your symptoms and whether they could point to fibromyalgia, multiple sclerosis (MS), or something else entirely.
Although fibromyalgia and MS sometimes look similar on the surface, they are very different conditions.
Fibromyalgia is a chronic pain disorder linked to how the brain processes pain signals. MS is an autoimmune disease that damages the nervous system. Understanding the differences matters because each condition requires a distinct approach to diagnosis and care.
This article breaks down the key differences and overlaps between fibromyalgia and MS, from causes and symptoms to diagnosis and treatment. You will also see how tools like the Human Health app’s symptom tracker can help you spot patterns and prepare for more productive conversations with your healthcare provider.
Fibromyalgia vs MS: The connection
Fibromyalgia and MS share several overlapping symptoms, such as fatigue, pain, and cognitive issues, but they are fundamentally different conditions.
Fibromyalgia is a chronic pain condition where the brain and nerves handle pain signals differently, but it doesn’t cause visible damage to the body’s nerves.
Multiple sclerosis, on the other hand, is an autoimmune disease where the immune system attacks the protective covering around nerves (called myelin). This attack leads to inflammation and lasting damage that can disrupt how the brain and body communicate.
Because some symptoms appear similar, this overlap may lead to confusion, delayed diagnosis, or even misdiagnosis. Recognizing the distinct nature of each condition is crucial for accurate treatment and effective long-term management.
Fibromyalgia vs MS: Key differences
Although they may share some overlapping symptoms, fibromyalgia and MS differ in several important ways:
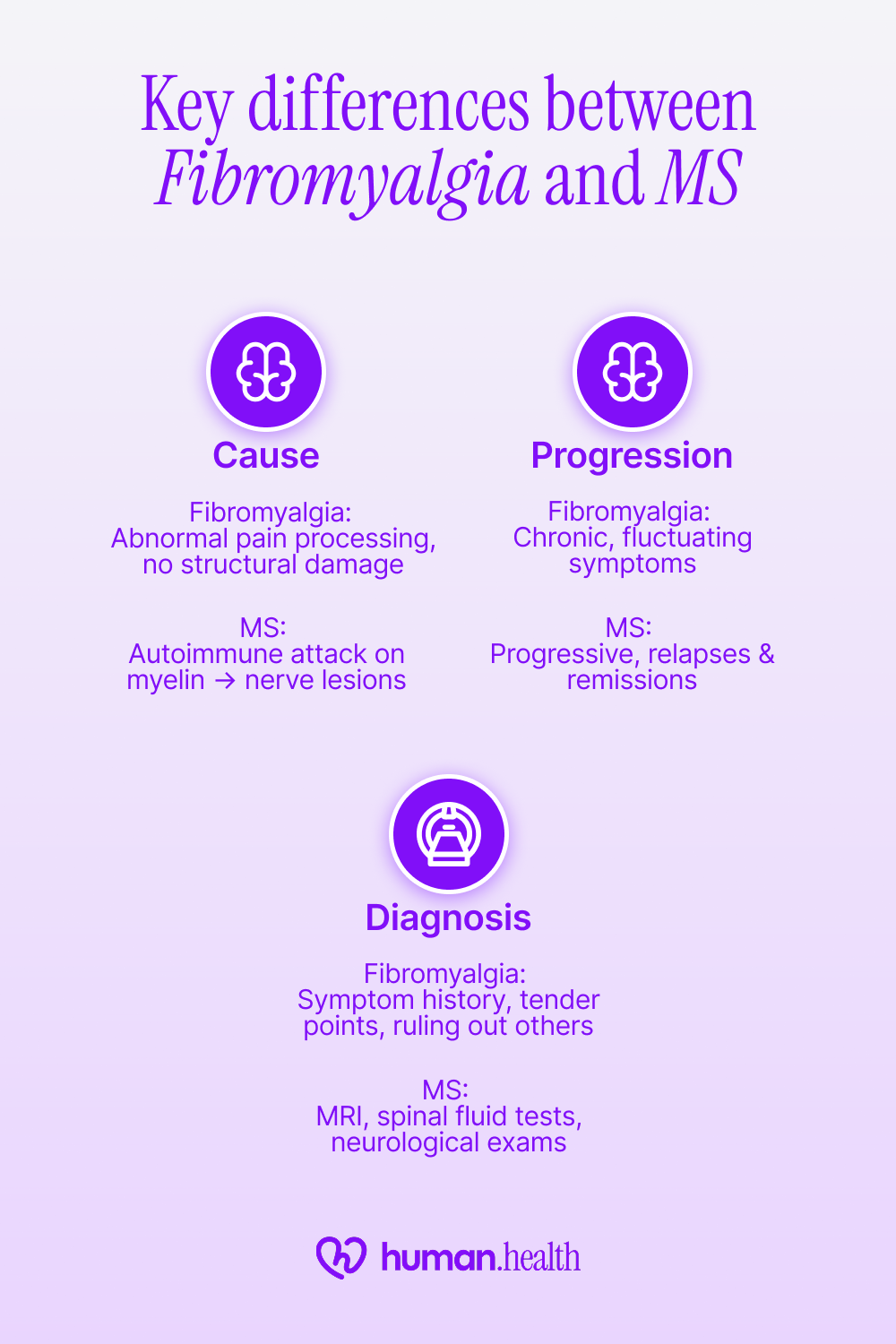
Cause
Fibromyalgia does not involve organic structural damage, but research suggests it is linked to abnormal pain processing and heightened sensitivity in the central nervous system.
In contrast, MS is caused by an autoimmune reaction in which the immune system mistakenly attacks the myelin sheath of nerve fibers (demyelination), causing lesions and disrupted communication between the brain and body.
Progression
Fibromyalgia is a chronic, non-degenerative condition in which symptoms may wax and wane over time, frequently influenced by stress, poor sleep, or lifestyle factors.
MS, however, follows a progressive course marked by relapses and remissions, and if not properly treated, can lead to lasting neurological disability.
Diagnostic tests
Fibromyalgia does not have a single test to confirm diagnosis. Instead, healthcare providers rely on symptom history, tender point evaluation, and ruling out other conditions.
You can, however, measure how fibromyalgia symptoms affect your daily life using the Fibromyalgia FIQR Test.
MS diagnosis, by comparison, uses objective tools such as MRI scans to detect brain and spinal cord lesions, spinal fluid analysis to reveal immune activity, and neurological exams to assess functional impact.
Together, these differences highlight why fibromyalgia and MS require very different diagnostic approaches and management strategies, even when their symptoms may initially look alike.
Symptom similarities of fibromyalgia and MS
Fibromyalgia and MS may coexist and share several common symptoms, which is why people sometimes confuse the two conditions. Understanding how these symptoms show up in each disorder can help highlight where the similarities end and the differences begin.
Fatigue
Fatigue is one of the most common symptoms in both fibromyalgia and MS, though how it feels and its triggers can differ by condition.
In fibromyalgia, fatigue is linked to poor sleep quality, chronic pain, and altered pain signaling, and it may also occur alongside other symptoms like nausea in fibromyalgia, dizziness, or headaches.
In MS, fatigue is neurological in origin and may be severe and overwhelming. In either case, this exhaustion can significantly interfere with work, relationships, and daily tasks.
Cognitive changes
Often called “fibro fog” in fibromyalgia or “MS cognitive dysfunction,” both conditions may affect memory, concentration, and the ability to process information. People may struggle with word recall, lose their train of thought, or feel mentally slower than usual.
These changes can be subtle or disruptive, making it difficult to distinguish which condition is driving them without medical evaluation.
Pain and sensory issues
Widespread pain is a hallmark of fibromyalgia, often described as muscle aches, joint stiffness, or tenderness throughout the body. MS, on the other hand, often causes neuropathic pain with sensations such as tingling, numbness, or burning in specific areas.
Despite these differences, the subjective experience of pain can feel similar, adding to the challenge of differentiating between the two.
You can learn more about fibromyalgia rib and chest pain and how it affects the body in our detailed guide.
Tracking how fatigue, brain fog, or pain change over time can bring clarity when symptoms overlap. The Human Health app’s symptom tracker makes it easier to spot trends and share them with your provider, giving you a clearer view of complex conditions like fibromyalgia and MS.
Can I have both fibromyalgia & MS?
Yes, it’s possible to be diagnosed with both fibromyalgia and MS, though it can be challenging to separate where one condition ends and the other begins.
MS is an autoimmune disease with identifiable nerve damage, while fibromyalgia is a pain-processing disorder without structural changes. Some people with MS also have fibromyalgia: studies show that the prevalence of fibromyalgia is significantly higher in the MS population than among those without MS.
Related overlaps, such as fibromyalgia and Autism, are also being studied to better understand shared neurological mechanisms and symptom patterns.
Because of the overlap, it’s especially important to work closely with a healthcare provider for an accurate diagnosis and treatment plan.
{{inline-cta-1}}
Possible causes of fibromyalgia and MS
Understanding what might cause fibromyalgia or MS can help explain why the two conditions are so different. While neither has a single clear cause, researchers have identified several factors that may play a role.
Fibromyalgia
Researchers have not identified a single cause of fibromyalgia, but possible contributors include:
- Abnormal pain processing in the brain and spinal cord
- Genetics and family history
- Physical or emotional trauma
- Sleep disturbances
- Co-existing conditions such as arthritis or mood disorders
MS
Multiple sclerosis is a disease in which the immune system attacks the central nervous system, causing immune-mediated inflammation and damage to myelin. Possible factors include:
- Immune system dysfunction (autoimmunity)
- Genetic predisposition
- Low vitamin D or reduced sun exposure
- Viral infections, such as Epstein-Barr virus
- Environmental and lifestyle influences
While researchers are still learning about both conditions, the main takeaway is that fibromyalgia and MS do not share the same root causes. Fibromyalgia is linked to how the body processes pain, while MS stems from immune system attacks on the nervous system. This difference explains why doctors take very different approaches to diagnosis and treatment.
How doctors diagnose fibromyalgia and MS
Getting the right diagnosis is often the hardest part, since fibromyalgia and MS share symptoms but require very different tests. Doctors use a mix of clinical evaluation, medical history, and (in the case of MS) imaging and lab work to tell them apart.
Fibromyalgia
Doctors diagnose fibromyalgia by evaluating symptoms and ruling out other conditions, since there’s no single test.
Diagnosis
- Based on widespread pain lasting at least three months
- Presence of associated symptoms such as fatigue, sleep disturbances, or cognitive issues
- Lab tests are often ordered only to exclude other causes, since imaging and labs are typically normal.
MS
Doctors usually confirm an MS diagnosis by identifying signs of nerve damage that appear in different parts of the central nervous system and at different points in time.
Diagnosis
Common tests include:
- MRI scans to look for lesions (areas of damage) in the brain or spinal cord
- Lumbar puncture to check spinal fluid for signs of immune activity
- Evoked potential tests to measure how quickly nerves respond to signals
Doctors use these results alongside the 2017 McDonald criteria, a set of guidelines designed to make MS diagnosis faster and more accurate.
Because symptoms overlap, misdiagnosis is common. Using the Human Health app’s symptom tracker to document fatigue, pain, or cognitive changes can provide a clear timeline that may support your conversations with healthcare providers.
Because fibromyalgia and MS share similarities with other conditions, including autoimmune diseases, it’s important to consider all possibilities.
Lupus, for instance, can also cause fatigue, brain fog, and widespread pain. You can take the short Lupus SLAQ Quiz to learn how lupus-related symptoms sometimes overlap and prepare for a more informed discussion with your healthcare provider.
Medications & treatment for fibromyalgia: What we know
Treatment for fibromyalgia focuses on reducing symptoms and improving quality of life rather than curing the condition.
What the research says
Research suggests several approaches may help manage fibromyalgia:
- A 2016 Cochrane review found that pregabalin may modestly reduce pain and improve other symptoms (including sleep) in some people with fibromyalgia.
- A 2021 randomized controlled trial found that regular aerobic-style exercise moderately improves fatigue (and may also reduce pain).
- Cognitive behavioral therapy (CBT) has shown modest benefits in helping people with chronic pain cope, improve pain, emotional distress, and quality of life.
Use the Human Health app's treatment log to record therapies and treatments. Over time, these records can help you and your healthcare provider see what is making a difference and adjust your plan more effectively.
Available MS treatments today: Backed by studies & data
MS treatments aim to slow disease progression, reduce relapses, and manage symptoms.
What the research says
Some medicines called disease-modifying therapies (DMTs) can help slow MS. Research shows they can lower the number of relapses and reduce new brain or spinal cord lesions seen on MRI scans. Starting stronger DMTs early may also help limit disability over the long term.
The Human Health medication tracker and symptom tracker can help you monitor how treatments affect relapses, fatigue, or pain. Sharing this information with your neurologist can make your appointments more effective.
Use the Human Health app to track your fibromyalgia and MS symptoms
Fibromyalgia and MS can share symptoms that blur the lines, but they remain very different conditions in origin, diagnosis, and treatment. Recognizing those differences is essential for getting the right care and for managing symptoms more effectively.
Tracking your health consistently is one of the best ways to bring clarity.
With the Human Health app, you can log flare-ups, treatments, and daily challenges in one secure place. You can also generate exportable PDF summaries to share with your healthcare provider, giving them a clearer view of your progress over time.
Explore the Human Health app today.
{{inline-cta-2}}
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- Medicine: Review of multiple sclerosis: Epidemiology, etiology, pathophysiology, and treatment
- National Library of Medicine: Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update
- Journal of Clinical Neurology: Current Updates on the Diagnosis and Management of Multiple Sclerosis for the General Neurologist
- ScienceDirect: Relapses in multiple sclerosis: Relationship to disability
- Sage Journals: Fatigue, depression, and pain in multiple sclerosis: How neuroinflammation translates into dysfunctional reward processing and anhedonic symptoms
- National Library of Medicine: Beyond pain in fibromyalgia: insights into the symptom of fatigue
- National Library of Medicine: Pathophysiology and Clinical Implications of Cognitive Dysfunction in Fibromyalgia
- National Library of Medicine: Cognitive Dysfunction in Multiple Sclerosis
- National Library of Medicine: Neuropathic Pain Secondary to Multiple Sclerosis: A Narrative Review
- National Library of Medicine: The incidence and prevalence of fibromyalgia are higher in multiple sclerosis than the general population: A population-based study
- Research, Society and Development: Genetic factors associated with fibromyalgia: a narrative review
- MDPI: Fibromyalgia: Understanding, Diagnosis and Modern Approaches to Treatment
- National Library of Medicine: Epstein-Barr virus, vitamin D and the immune response: connections with consequences for multiple sclerosis
- National Library of Medicine: Environmental and genetic risk factors for MS: an integrated review
- National Library of Medicine: Risk factors for multiple sclerosis in the context of Epstein-Barr virus infection
- National Library of Medicine: Lifestyle and Environmental Factors in Multiple Sclerosis
- Medscape: Fibromyalgia Clinical Presentation
- Medscape: Multiple Sclerosis Workup
- National Library of Medicine: Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria
- Cochrane: Pregabalin for treating fibromyalgia pain in adults
- ScienceDirect: Effectiveness of Exercise on Fatigue and Sleep Quality in Fibromyalgia: A Systematic Review and Meta-analysis of Randomized Trials
- Frontiers in Psychology: A systematic review of cognitive behavioral therapy-based interventions for comorbid chronic pain and clinically relevant psychological distress
- Frontiers in Psychology: Therapeutic Advances in Multiple Sclerosis
- MS Brain Health: Evidence for the benefit of early treatment in MS – what’s new?
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Track The Symptoms of Your Condition In Our App!
Inside the Human Health app - you can track all your symptoms, for multiple conditions. This allows you to have a centralized view of your condition(s) in one place, and gain insights.
See the Full Picture of Your Health
With the Human Health app, you can track symptoms for every condition and spot insights that help you take action.







.jpg)





.png)

