Fibromyalgia and Neuropathy: Links, Symptoms & Differences
October 12, 2025

- Fibromyalgia and neuropathy share similar symptoms, including pain, tingling, fatigue, and sleep disruption, but they have different underlying causes.
- Neuropathy usually involves measurable nerve damage, while fibromyalgia is a chronic pain condition that affects how the brain and nerves process pain signals.
- Some research suggests a subset of people with fibromyalgia may also show small fiber neuropathy, but the link is still being studied.
- Tracking symptoms over time can help you and your healthcare provider identify whether changes relate more to nerve damage or widespread pain sensitivity.
Disclaimer: This article is for informational purposes only and is not a substitute for medical advice, diagnosis, or treatment. Always seek advice from a qualified healthcare provider for any medical concerns.
If you live with ongoing pain, tingling, or exhaustion, it can be hard to tell what’s really behind it. For many people, fibromyalgia and neuropathy can feel almost identical at first: both can cause burning sensations, numbness, or deep aching that disrupts daily life.
Yet beneath those shared symptoms lie two very different stories.
Fibromyalgia affects how your nervous system processes pain, while neuropathy involves damage to the nerves themselves.
This article explores how the two conditions may overlap, what sets them apart, and what current research suggests about possible connections. You’ll also find ways to observe patterns, manage symptoms more confidently, and track your experiences using the Human Health app.
What is neuropathy and how might it differ from fibromyalgia?
Neuropathy refers to damage or dysfunction in the nerves that carry messages between the brain, spinal cord, and the rest of the body. It can cause sensations such as tingling, numbness, burning pain, or weakness, often starting in the hands or feet.
Fibromyalgia, on the other hand, doesn’t cause physical nerve damage. Instead, it affects how the brain and spinal cord process pain signals, which can make ordinary sensations feel more intense. Many people describe widespread muscle pain, deep fatigue, sleep disruption, and periods of mental fogginess (often called “fibro fog”).
Because both can cause pain and sensitivity, the differences are not always clear. This overlap can make diagnosis challenging, especially when symptoms vary from day to day.
Could fibromyalgia possibly cause neuropathy or be linked to nerve damage?
Fibromyalgia is not traditionally classified as a nerve damage disorder. However, some studies suggest there may be a possible link between fibromyalgia and small fiber neuropathy, a condition that affects the tiny nerve fibers responsible for sensing pain and temperature.
Recent studies show that around half of people with fibromyalgia have a mild reduction in small nerve fibers in the skin. Researchers continue to debate whether this finding helps explain symptoms like tingling or burning pain, or whether it reflects a separate process that sometimes occurs alongside fibromyalgia.
What symptoms might overlap between neuropathy and fibromyalgia?
Because fibromyalgia and neuropathy both affect how the body senses and responds to pain, their symptoms can look similar. Here’s how some of the most common symptoms might overlap and differ between the two conditions.
{{inline-cta-1}}
Pain
Pain is central to both conditions, but it originates differently. In neuropathy, pain typically results from nerve damage and is often described as sharp, burning, or shooting sensations, usually affecting the hands or feet. In fibromyalgia, pain is widespread (affecting muscles and soft tissues) and driven more by alterations in how the brain and spinal cord process pain (central sensitization) rather than overt nerve damage.
You can learn more about Fibromyalgia Breast & Armpit Pain and how it relates to widespread pain symptoms in our detailed guide.
Tingling and numbness
Both neuropathy and fibromyalgia can cause tingling or pins and needles sensations, but for different reasons. In neuropathy, this often happens because the nerves that send messages to your brain are damaged or irritated. In fibromyalgia, tingling can appear even when tests show no nerve injury. It may stem from the body’s heightened sensitivity to normal signals rather than from nerve damage itself.
Fatigue and sleep disturbance
Feeling drained or unrested is common in both neuropathy and fibromyalgia. In neuropathy, ongoing burning or tingling pain can make it hard to fall or stay asleep. In fibromyalgia, fatigue often stems from poor-quality, non-restorative sleep and the way the brain processes pain signals. In both conditions, lack of rest can heighten pain and make it harder to cope day to day.
Recognizing where these symptoms overlap can make it easier to discuss patterns with your healthcare provider and determine whether nerve testing or other evaluations might help clarify what’s going on.
{{pro-tip-1}}
How common might neuropathy be in people with fibromyalgia?
Researchers have looked closely at whether fibromyalgia might involve tiny changes in the nerves that sense pain and temperature. A large 2022 review of 20 studies found that around half of people with fibromyalgia showed signs of small fibre impairment when tested using skin biopsies or imaging of the cornea.
However, this does not mean that fibromyalgia is caused by nerve damage. Many people with fibromyalgia have completely normal nerve tests. These results mainly suggest that, for some, subtle changes in small nerve fibres could add to their pain experience. Experts agree that more research is needed to understand exactly how (or if) these findings are connected to the condition itself.
Could neuropathy symptoms possibly make fibromyalgia worse?
Neuropathy and fibromyalgia can influence each other in complex ways. Because neuropathic pain involves central sensitization mechanisms, burning or tingling from neuropathy may further engage shared central amplification circuits, potentially heightening pain sensitivity in someone with fibromyalgia. Similarly, fibromyalgia’s characteristic fatigue, sleep disruption, and stress-related sensitization may amplify the subjective intensity of nerve-related pain.
This interaction can create a vicious cycle where poor sleep, pain flare-ups, and exhaustion feed into one another. Tracking symptoms may help identify triggers and patterns that worsen pain over time.

What tests might help distinguish neuropathy from fibromyalgia?
Doctors use different tests because these conditions affect the body in different ways. Neuropathy is usually checked through tests that measure how well the nerves are working. These may include nerve conduction studies or electromyography (EMG) to look for larger nerve damage, and sometimes a small skin sample (biopsy) to check for changes in tiny nerve fibers.
Fibromyalgia, on the other hand, does not show nerve damage on these tests. Diagnosis is based on your symptoms, a physical exam, and ruling out other possible causes. Keeping track of your symptoms and patterns can help your healthcare provider make a clearer, more accurate assessment.
If you’d like to reflect on how fibromyalgia may be affecting different areas of your daily life, the Fibromyalgia FIQR Quiz offers a simple way to explore your current symptom patterns before your next healthcare appointment.
How to manage both fibromyalgia and neuropathy

Living with fibromyalgia and neuropathy can mean navigating overlapping symptoms and unpredictable energy levels. While approaches differ for everyone, observing how your body responds to certain habits can help you make informed choices and have clearer discussions with your healthcare provider.
Gentle movement
Some people find that light, regular physical activity, such as gentle walking, stretching, or low-impact exercises, helps reduce stiffness and support circulation when done within personal limits. Tracking how your body feels after each type of movement can reveal what’s tolerable and what feels too demanding.
{{pro-tip-2}}
Energy pacing
Both conditions can involve fluctuating fatigue. Planning lighter tasks between more demanding ones, or spreading activities across several days, may help reduce the strain that can lead to flare-ups. Over time, pattern tracking can help you understand how your energy changes day to day.

Sleep support
Poor sleep can intensify pain and fatigue by lowering the pain threshold and increasing pain sensitivity. Noting bedtime routines, nighttime pain, and how refreshed you feel in the morning can help highlight what improves rest. Some people find that relaxing activities or a consistent routine make a difference, while others may need to discuss ongoing sleep problems with their healthcare provider.
Stress awareness
Stress can make pain feel stronger in both fibromyalgia and neuropathy. Studies show that when people with fibromyalgia experience stress, their sensitivity to pain often increases. Noticing emotional triggers and building calming routines, such as journaling, deep breathing, or quiet hobbies, may help reduce flare-ups. Over time, understanding which situations raise or ease stress can make it easier to manage symptoms day to day.
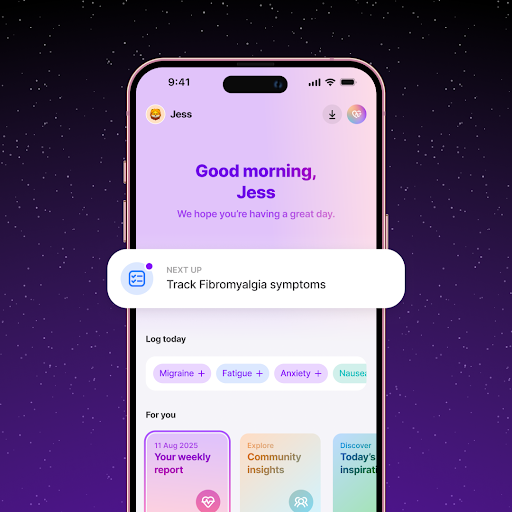
Tracking and reflection
Using the Human Health app can help you notice subtle changes in pain, sleep, or fatigue patterns. Over weeks or months, these logs can show whether certain routines, foods, or stress levels coincide with better or worse symptom days, giving you and your healthcare provider clearer insight into potential triggers.
When should you see a doctor?
It can be difficult to know when to seek medical advice, especially when symptoms come and go. However, it’s important to reach out to a healthcare provider if you notice new sensations such as burning, numbness, or weakness that persist or worsen over time.
If your pain begins to interfere with daily activities, sleep, or emotional well-being, a doctor can help rule out other causes and recommend further testing if needed. Bringing a record of your symptoms (including timing, intensity, and possible triggers) can help make the conversation more focused and productive.

Spot symptom patterns in fibromyalgia and neuropathy with the Human Health app
Both fibromyalgia and neuropathy can fluctuate from day to day, making it hard to see what truly influences pain, fatigue, or energy. Tracking these changes helps you uncover patterns that aren’t always obvious in the moment.
With the Human Health app, you can log symptoms, treatments, and energy levels, then review how they shift over time. This makes it easier to discuss what’s helping, what’s not, and where to focus next with your healthcare provider.
Understanding your symptoms is the first step to managing them. The Human Health app helps you see your progress, recognize what shapes your pain and energy, and take an active role in your own care.
{{inline-cta-2}}
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- National Institute of Neurological Disorders and Stroke: Peripheral Neuropathy
- National Library of Medicine: The Science of Fibromyalgia
- National Library of Medicine: Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia
- National Library of Medicine: Small fiber pathology in fibromyalgia syndrome
- National Library of Medicine: Central sensitivity and fibromyalgia
- Frontiers in Molecular Neuroscience: Peripheral mechanisms of peripheral neuropathic pain
- PAIN Reports: Distinguishing fibromyalgia syndrome from small fiber neuropathy: a clinical guide
- National Library of Medicine: Sleep disorders in chronic pain and its neurochemical mechanisms: a narrative review
- National Library of Medicine: Sleep Disturbances in Fibromyalgia Syndrome: Relationship to Pain and Depression
- National Library of Medicine: A Systematic Review and Meta-Analysis of the Prevalence of Small Fibre Impairment in Patients with Fibromyalgia
- National Library of Medicine: Nociplastic pain and central sensitization in patients with chronic pain conditions: a terminology update for clinicians
- Cleveland Clinic Journal of Medicine: Central sensitization, chronic pain, and other symptoms: Better understanding, better management
- National Library of Medicine: A Systematic Review of the Diagnostic Methods of Small Fiber Neuropathies in Rehabilitation
- Wiley Online Library: Effectiveness of Therapeutic Exercise in Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis of Randomized Clinical Trials
- National Library of Medicine: Chronic pain management and sleep disorders
- PLOS One: Stress-Induced Allodynia – Evidence of Increased Pain Sensitivity in Healthy Humans and Patients with Chronic Pain after Experimentally Induced Psychosocial Stress
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Track Your Health Daily
Keep a record of your symptoms, treatments, and daily progress with helpful reminders from the Human Health app.

Keep Your Wellness in Check
From symptom logging to treatment reminders - manage your health confidently with the Human Health app.






Pro tip
Keep a timeline, not just a checklist.
When you’re tracking fibromyalgia or neuropathy symptoms, note when they appear and what happened beforehand (for example, stress, activity, temperature, or sleep quality.) Patterns often emerge over weeks rather than days, helping you and your clinician see connections that single symptom lists can miss.
Pro tip
Pay attention to early body cues.
Some people living with fibromyalgia or neuropathy notice that tingling, burning, or other sensory changes appear before pain or fatigue worsens. Tracking these shifts over time can help you spot your own patterns and plan rest or activity in a way that feels more manageable.

.jpg)





.png)

