Fibromyalgia Numbness: Causes, Relief Tips & Advice
August 21, 2025

- Numbness and tingling affect most people with fibromyalgia, often shifting in location and intensity.
- Research links these sensations to small-fiber neuropathy, central sensitisation, and nervous system changes.
- Symptoms may not follow typical nerve patterns and can appear in various body areas, sometimes without clear triggers.
- Tracking when, where, and how symptoms change can help you and your clinician find better management strategies.
- The Human Health app offers an interactive way to log and visualise these patterns over time.
Disclaimer: Human Health is not recommending any specific medical treatment for any particular symptom, nor providing any other medical advice. Always seek the advice of your doctor or healthcare provider regarding any medical concern.
If you live with fibromyalgia, you might know the strange mix of surprise and frustration that comes with sudden numbness or tingling. One moment you feel fine, and the next, part of your body feels dull, heavy, or oddly “asleep”. Sometimes for minutes, sometimes for hours.
These sensations are a familiar part of life for many people with fibromyalgia, but they can still be unsettling. In this article, we’ll look at why they happen, which areas are most often affected, how to spot when it could be something else, and ways to track and talk about them with your healthcare provider.
What is fibromyalgia numbness & why does it happen
Numbness and tingling are among the less-understood symptoms of fibromyalgia. Often described as a loss of sensation, a “pins and needles” feeling, or skin that feels oddly thick, this experience is known medically as paresthesia.
Researchers haven’t pinpointed a single cause, but it’s thought to be linked to changes in how the brain and nervous system process pain and sensory signals. These altered pain pathways can make harmless sensations feel unusual, uncomfortable, or even alarming, similar to the sensory processing differences sometimes observed in fibromyalgia and autism. For some, numbness appears alongside other fibro symptoms such as fatigue or muscle stiffness, and it may come and go without a clear trigger.
For some, numbness appears alongside other fibro symptoms such as fatigue or muscle stiffness, and it may come and go without a clear trigger.
You can learn more about related symptoms such as Fibromyalgia Breast & Armpit Pain and how they connect to the body’s complex pain responses.
Possible causes of fibromyalgia numbness
Numbness and tingling are widely reported in fibromyalgia, with studies finding them in a majority of patients (research suggests anywhere from around two-thirds to over 80%). While the exact reason isn’t always clear, research points to a few possible factors
- Central sensitization: An over-responsive nervous system can amplify ordinary sensations, making them feel strange or uncomfortable. This process has been seen in brain imaging and sensory testing in people with fibromyalgia.
- Small-fiber nerve changes: In some cases, tiny sensory nerve fibers in the skin show changes linked to fibromyalgia. Multiple studies using skin biopsy and sensory testing suggest that around 40% of people with fibromyalgia meet criteria for small-fiber neuropathy, which can cause numbness and tingling.
- Objective neurological changes: Controlled studies have found that self-reported numbness often matches up with measurable differences on neurological exams, supporting the idea that these sensations have a physical basis.
- Symptom clustering: Numbness often appears alongside fatigue, poor sleep, and other fibro symptoms, suggesting it may be part of a broader pattern rather than a stand-alone issue.
{{pro-tip-1}}
Common symptoms and affected areas
Many people with fibromyalgia report sensations such as numbness or tingling, sometimes described as pins and needles. Neurological studies suggest these feelings may affect different areas of the body rather than following one specific nerve path.
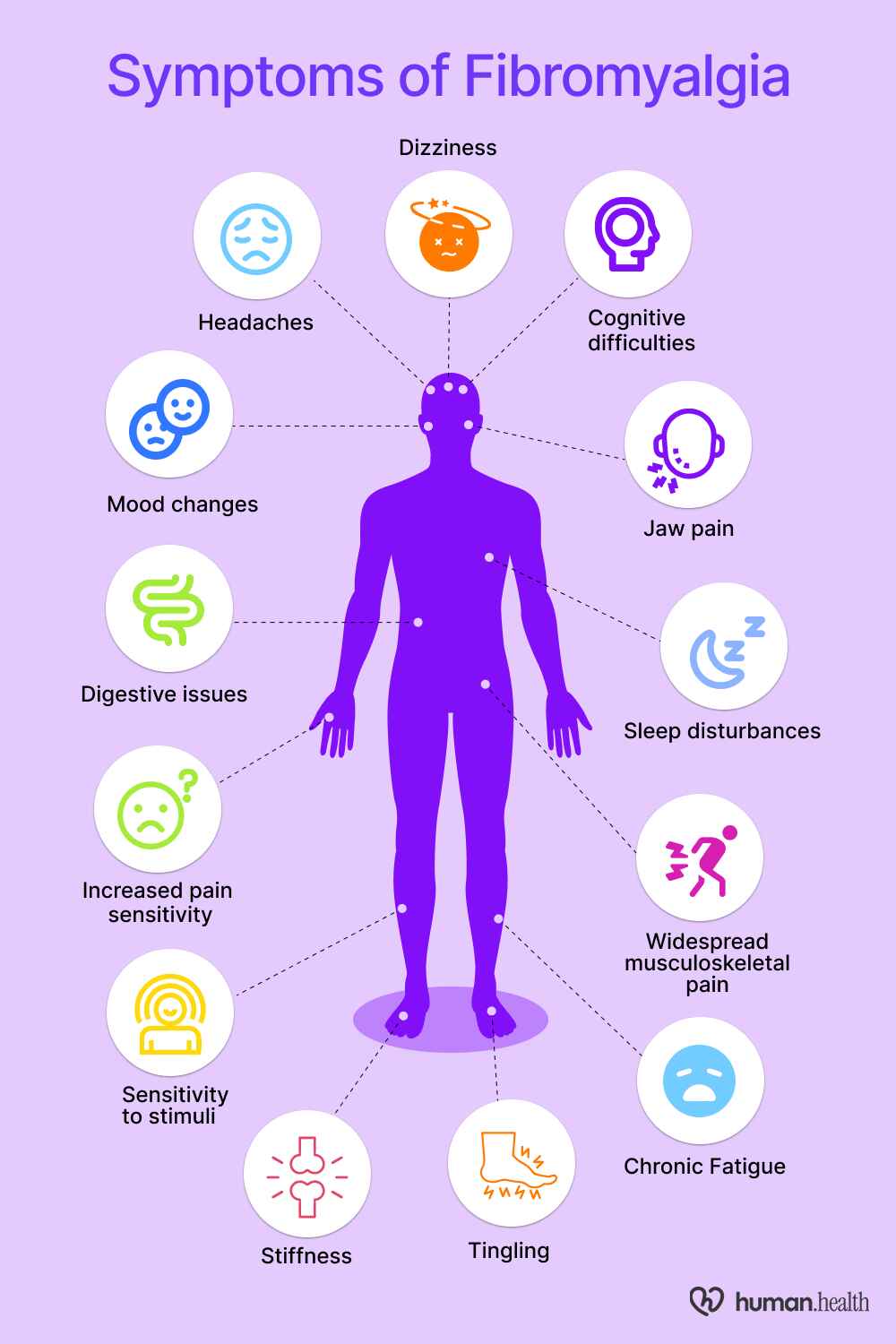
Hands and fingers
Fibromyalgia frequently causes numbness or tingling in the hands and arms (along with fingers), sometimes affecting both sides or one more than the other. These altered sensations can make fine motor tasks (like writing or buttoning clothing) more difficult.
Feet and toes
Numbness, tingling, or heaviness in the feet and toes are also commonly reported symptoms in fibromyalgia. These sensations may not follow specific nerve pathways and can come and go unpredictably. Some people notice that the discomfort worsens after long periods of standing or remaining still.
Arms and legs
Studies have found that tingling or numbness can appear in both the arms and legs for some people with fibromyalgia. These sensations may come and go, change in strength, or move between different areas of the body without a clear pattern.
Face/facial regions
Though less common, facial numbness or tingling has been observed in fibromyalgia, often linked with dental or jaw discomfort. The condition’s sensory changes can involve the cheeks, lips, or jaw areas.
You can learn more about the connection between TMJ and Fibromyalgia and how jaw-related pain may contribute to facial discomfort.
Shifting and fluctuating patterns
Fibromyalgia symptoms (including numbness) may shift unpredictably in location and intensity. Patients report that these sensations can appear or fade without any clear cause. This unpredictability makes it difficult to identify consistent triggers or patterns over time.
This unpredictability extends to various sensations, leading many to ask if itching is a fibromyalgia symptom as well.
{{pro-tip-3}}
Is the numbness caused by fibromyalgia or something else?
Although numbness and tingling are common in fibromyalgia, they can also be linked to other health conditions. In fact, some people initially confuse the symptoms with those of other chronic pain disorders, which is why understanding the differences between conditions such as polymyalgia rheumatica and fibromyalgia, and osteoarthritis and fibromyalgia is essential. These conditions may have overlapping symptoms but very different underlying causes and treatments, making it important to review all possibilities with your healthcare provider.
Carpal tunnel syndrome
This condition occurs when the median nerve is compressed as it passes through the wrist. It can cause numbness, tingling, and weakness in the hand and fingers (often the thumb, index, and middle fingers). Symptoms may worsen at night or after repetitive hand use.
Peripheral neuropathy
Peripheral neuropathy happens when nerves outside the brain and spinal cord are damaged, sometimes due to diabetes, vitamin deficiencies, or certain medications. It can cause numbness, burning, or tingling in the hands and feet, often following a “stocking-glove” pattern.
You can learn more about the connection between Fibromyalgia and Neuropathy to understand how nerve pain and sensitivity may overlap in both conditions.
Multiple sclerosis (MS)
MS is an autoimmune condition that affects the central nervous system. Numbness can be one of the earliest symptoms, appearing in the face, limbs, or trunk. It often occurs alongside other neurological signs, such as vision changes, muscle weakness, or balance problems.
Cervical or lumbar spine issues
Numbness can also happen when a spinal nerve is compressed, such as from a slipped disc, spinal narrowing, or age-related changes in the neck or lower back. In these cases, the tingling or numbness usually follows a specific path, like down one arm or leg.
Top tip: If you notice that numbness follows a consistent path or is always in the same area, this is important to share with your healthcare provider, as it may point to a structural nerve issue rather than fibromyalgia.
{{inline-cta-1}}
Migraine with sensory aura
In some migraine attacks, temporary sensory symptoms like tingling or numbness may occur, sometimes involving the face, arms, or hands, and typically evolve gradually over minutes and resolve within about an hour.
{{pro-tip-2}}
Tips & treatments to manage fibromyalgia numbness
While there’s no single fix for fibromyalgia numbness, there are ways to make it less disruptive day to day. These strategies focus on comfort, mobility, and better understanding your symptoms over time, and may complement other approaches such as exploring natural remedies for fibromyalgia, and new treatment for fibromyalgia.
Gentle movement and stretching
For people with fibromyalgia, low-impact activities such as walking, swimming, or gentle yoga may support overall movement and comfort. Light stretching, especially in areas that feel numb or tense, can also help maintain flexibility and keep joints and muscles moving more easily.
Temperature therapy
Alternating warm and cold compresses may enhance circulation and nerve responsiveness in affected areas. Warm baths or showers are often reported to help 'wake up' numb regions.
Posture adjustments
Because poor posture or repetitive strain can place pressure on peripheral nerves (e.g. in the neck, shoulders, or back), using an ergonomic setup and taking posture breaks may reduce symptom burden.
Nerve-friendly nutrition
Emerging evidence suggests that maintaining adequate vitamin B12 (and related nutrients) may support nerve and fibromyalgia health. Always confirm supplements or dietary changes with a healthcare provider before starting.
Stress management techniques
Stress may worsen fibromyalgia symptoms (potentially including numbness). Clinical evidence indicates that mindfulness meditation and related mind-body practices may reduce symptom severity and psychological distress.
“The most significant improvements come from lifestyle changes. Programs that blend psychological and physical therapy methods have shown substantial benefits. These programs emphasise the importance of pacing oneself, finding a balance in activities, and altering attitudes toward rest.”- Dr Rafik Sedra, Consultant in Pain Medicine and Anaesthesia.
Top tip: Use the Human Health app’s guided routines and sleep tracker to build habits that support symptom management. By logging daily activities and symptoms, you can start to see what’s helping and what might be making numbness worse.
When to seek medical advice
Numbness with fibromyalgia is often harmless, but there are times when you should get it checked promptly. Because numbness can also be a symptom of other conditions (such as nerve compression, multiple sclerosis, or peripheral neuropathy), it’s important not to assume it’s always linked to fibromyalgia.
Seek medical advice if you notice:
- Sudden onset of numbness or tingling, especially on one side of the body.
- Progressive worsening over days or weeks.
- Accompanying weakness, vision changes, loss of balance, or difficulty speaking.
- Persistent numbness that does not improve with your usual self-management strategies.
Your clinician may recommend neurological tests, blood work, or imaging to rule out other causes before confirming a fibromyalgia-related origin.
{{pro-tip-4}}
How the Human Health app can help you track and manage fibromyalgia symptoms
Keeping track of when and where numbness occurs can reveal valuable patterns. Patterns that may be hard to spot day-to-day. The Human Health app lets you log symptoms in real time and record details such as the location, type, and intensity of each Fibromyalgia flare-up. You can also log related sleep symptoms or note activities within your plan that might influence how you feel. Over time, these insights can help you and your clinician refine your management plan.
If you’re curious how your overall symptoms compare to others with fibromyalgia, the Fibromyalgia FIQR Test can help you understand the impact of your symptoms and guide what to discuss with your healthcare provider.
Start tracking your symptoms today.
FAQs:
#1. Can fibromyalgia numbness become permanent?
It’s usually temporary and fluctuates. Long-term numbness is uncommon and may signal another condition, so it’s worth discussing with your doctor.
#2. Should I be concerned if it’s only on one side of the body?
Yes. While fibromyalgia symptoms can be patchy, numbness on one side should be checked to rule out other neurological causes.
#3. What’s the difference between numbness and tingling in fibromyalgia?
Numbness is reduced sensation; tingling is a “pins and needles” feeling. Both can occur together in fibromyalgia due to altered nerve signalling.
Disclaimer: Human Health is not recommending any specific medical treatment for any particular symptom, nor providing any other medical advice. Always seek the advice of your doctor or healthcare provider regarding any medical concern.
Sources:
- PubMed Central: Neurological signs and symptoms in fibromyalgia
- The Lancet Rhematology: Central sensitisation in chronic pain conditions: latest discoveries and their potential for precision medicine
- PubMed Central: Specific symptoms may discriminate between fibromyalgia patients with vs without objective test evidence of small-fiber polyneuropathy
- Frontiers in Medicine: Fibromyalgia and Associated Disorders: From Pain to Chronic Suffering, From Subjective Hypersensitivity to Hypersensitivity Syndrome
- National Library of Medicine: Carpal Tunnel Syndrome
- National Institute of Neurological Disorders and Stroke: Peripheral Neuropathy
- National Institute of Neurological Disorders and Stroke: Multiple Sclerosis
- Arthritis Foundation: Can Fibromyalgia Cause Numb Feet?
- UW Orthopaedic Surgery and Sports Medicine: Fibromyalgia
- National Library of Medicine: Lumbosacral Radiculopathy
- National Library of Medicine: Chapter 51 Episodic Neurologic Symptoms
- ScienceDirect: Physical activity in the treatment of fibromyalgia
- BMC: Multimodal non-invasive non-pharmacological therapies for chronic pain: mechanisms and progress
- ResearchGate: Influence of ergonomic factors on peripheral neuropathy under HAV exposure
- National Library of Medicine: Neuronutritional Approach to Fibromyalgia Management: A Narrative Review
- Pain Physician Journal: Mindfulness Meditation for Fibromyalgia Syndrome: A Systematic Review and Meta-analysis
- NHS: Fibromyalgia Symptoms
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Try The Human Health App For Free Today
Track symptoms, log your medications, appointments and more!







Pro tip
Log when numbness happens, what you're doing, and how long it lasts in the Human Health app. These patterns can help you and your healthcare provider better understand what’s going on.
Pro tip
Use the symptom tracking feature in the Human Health app to record the type, intensity, and frequency of numbness. You can then add a journal entry alongside it to capture extra context (for example, noting if headaches, posture changes, or specific activities occurred at the same time). This combination can give your healthcare provider a clearer picture of patterns over time.
Pro tip
Tracking numbness in the Human Health app helps you record exactly where and when symptoms appear. Over time, this can make it easier to spot trends, triggers, or patterns to share with your healthcare provider.
Pro tip
Bring the Human Health app’s symptom log to your appointment. It can give your clinician a clear timeline of when numbness began, how it has changed, and whether it links to activity, sleep, or stress patterns.

.jpg)





.png)

