Osteoarthritis and Fibromyalgia: Overlaps & How to Manage
October 1, 2025
- You can have both conditions: Osteoarthritis (OA) affects the joints, while fibromyalgia causes widespread pain, fatigue, and sensitivity - some people live with both.
- Similar symptoms can blur the picture: Joint stiffness from OA and whole-body pain from fibromyalgia often overlap, making it harder to know what’s causing what.
- Symptom tracking, gentle activity, stress management, and medical support together may help you feel more in control day-to-day.
- Your healthcare provider is essential: Seeing a doctor early can help you get a clear diagnosis and a personalized plan that fits your needs.
Disclaimer: Information in this article is for general education only. Human Health is a tracking and support tool and does not provide medical advice, diagnosis, or treatment. Always talk to a qualified healthcare provider about your health.
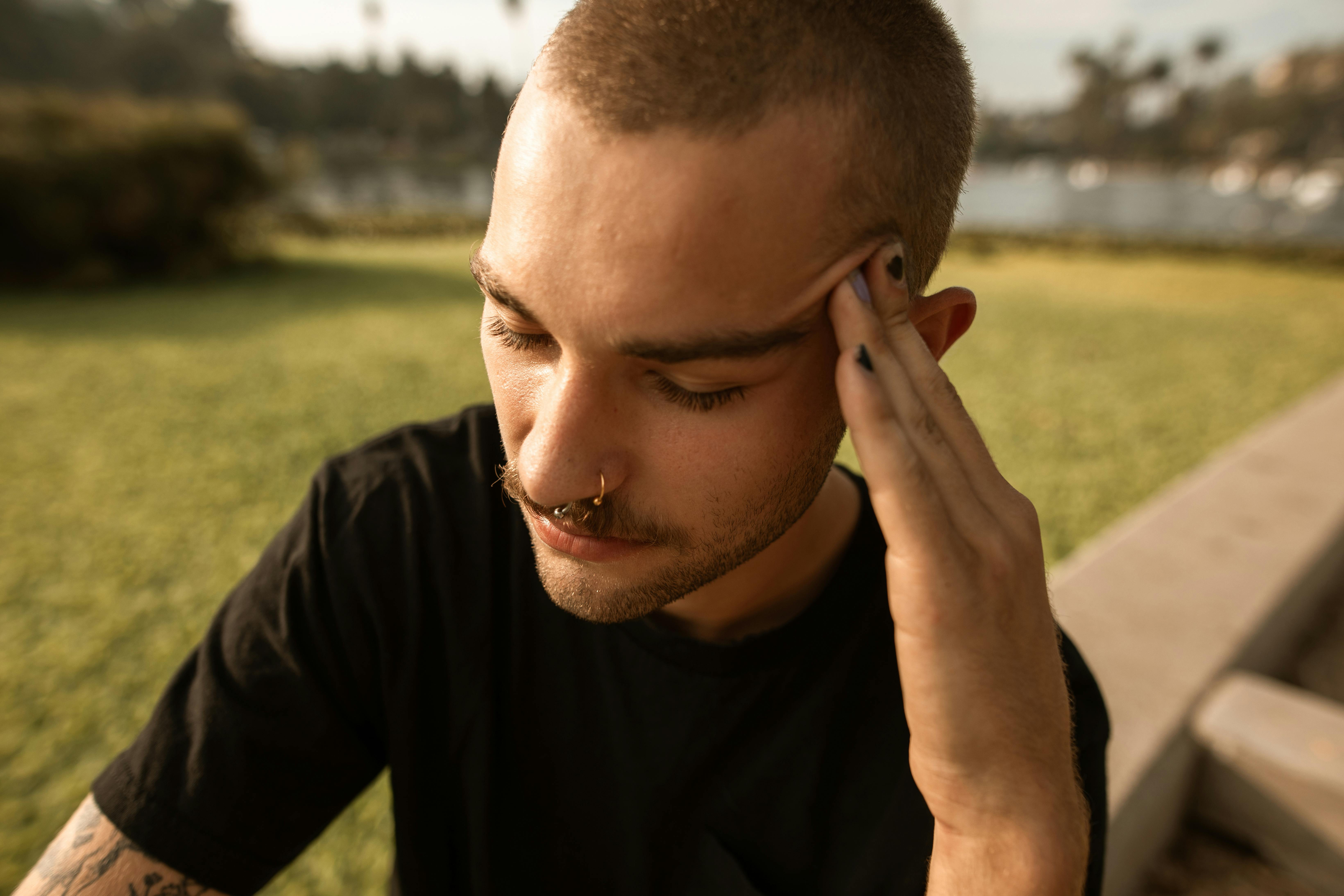
Living with daily aches, stiffness, or exhaustion can be confusing. Some days it feels like your joints are the problem, other days it’s pain all over, and sometimes it’s both. That uncertainty alone can take a toll.
Osteoarthritis and fibromyalgia often overlap, which makes it harder to know what’s happening or how to explain it. You are not alone. Many people face both conditions at the same time.
In this guide, we’ll look at how the two differ, where they overlap, and what patterns to track so you and your healthcare provider can get a clearer view. You’ll also see how the Human Health app helps you log symptoms, spot trends, and feel more supported in daily life.
Osteoarthritis and Fibromyalgia: What to know
Osteoarthritis and fibromyalgia are two different conditions, but both can cause ongoing pain and limit daily activities. Understanding what each one is helps explain why their symptoms sometimes overlap.
What is osteoarthritis?
Osteoarthritis (OA) is the most common type of arthritis and develops when joints gradually break down, most often in the hands, hips, back, or knees. It can cause joint pain, swelling, stiffness, and reduced mobility, sometimes making daily activities harder to manage.
What is fibromyalgia?
Fibromyalgia is a chronic pain disorder primarily characterized by widespread musculoskeletal pain, often accompanied by fatigue, cognitive dysfunction (commonly described as ‘brain fog’), and sleep disturbances. Unlike osteoarthritis, fibromyalgia does not result from joint damage but from altered pain regulation in the central nervous system, a process known as central sensitization.
Can you have osteoarthritis and fibromyalgia at the same time?
Yes, fibromyalgia can coexist with osteoarthritis. In fact, research shows that fibromyalgia is diagnosed in over one-third of knee OA patients, and when both conditions occur together, their overlapping symptoms can further affect pain, function, and quality of life.
People who have both may experience joint pain and stiffness from OA, along with widespread pain, fatigue, and brain fog from fibromyalgia. This overlap can make it harder to know which condition is behind a particular symptom.
Recognizing that you may have both is important because it helps you and your healthcare provider create a more tailored plan for treatment and daily management.
Risks of having osteoarthritis and fibromyalgia
Living with two chronic pain conditions at once can amplify the burden. When osteoarthritis and fibromyalgia overlap, the combined symptoms can put more pressure on mobility, energy, and emotional resilience, making everyday life more of a balancing act.
Understanding the possible risks of managing both together can help you prepare and feel more in control.
Added pain and fatigue
When OA’s joint pain and fibromyalgia’s widespread sensitivity join forces, they can lead to more intense discomfort and exhaustion. In people with osteoarthritis, pain contributes significantly to fatigue, which in turn can worsen pain perception and limit function.
Reduced ease of movement
Joint stiffness from OA and tenderness or muscle pain from fibromyalgia can make movement harder. In fibromyalgia, especially, pain and fatigue together explain a large share of the reduction in physical performance and how well people believe they can move.
Impact on mood and rest
When pain is relentless and sleep suffers, mood often takes a hit. In fibromyalgia and OA, worsening pain severity is closely tied to poorer sleep quality, and both contribute to declines in mood and emotional health.
Together, these risks can feel overwhelming, but they also highlight why clear tracking matters. Recording changes in pain, sleep, and energy can give you and your healthcare provider a fuller picture, making it easier to adjust care and find strategies that support your daily life.
How to tell the difference between osteoarthritis and fibromyalgia symptoms
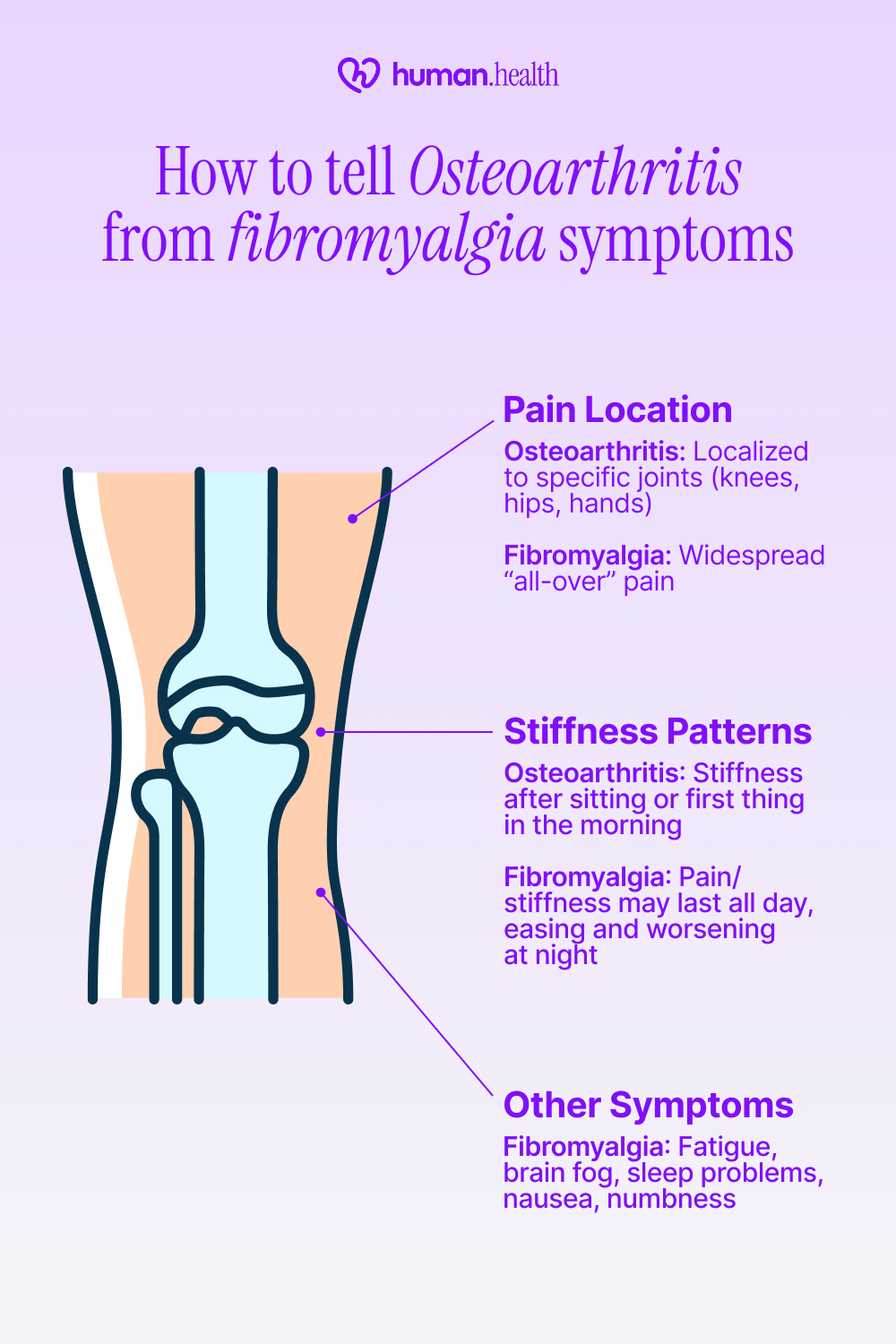
Both conditions can cause ongoing pain and stiffness, which makes it hard to know which one is at play. Understanding a few key differences can help you notice patterns to share with your healthcare provider.
- Pain location: Osteoarthritis pain typically settles in specific joints, such as your knees, hips, or hands. Fibromyalgia pain is more widespread and may feel like it’s “all over.” This difference matters because localized joint pain may limit certain movements, while widespread pain can drain overall energy.
- Stiffness patterns: With OA, stiffness often flares after sitting still or first thing in the morning. In fibromyalgia, some people feel pain and stiffness all day, while others notice it easing and then worsening again at night. These patterns shape how predictable or unpredictable the day feels.
- Other symptoms: Fibromyalgia often brings fatigue, brain fog (cognitive dysfunction), and sleep problems, features not typical in osteoarthritis. Some individuals also experience fibromyalgia nausea or even fibromyalgia numbness, which can further affect appetite, comfort, and overall energy levels throughout the day. If you notice a mix of these signs, avoid self-diagnosis. Sharing a symptom log with your healthcare provider gives them a clearer picture to work with.
If you’re noticing ongoing joint pain, fatigue, or stiffness that don’t quite fit the pattern of osteoarthritis or fibromyalgia, it may be helpful to explore whether another condition could be contributing. Autoimmune conditions such as lupus can sometimes mimic these symptoms. You can take the Lupus SLAQ Quiz to better understand your symptom patterns before talking with your healthcare provider.
If lupus is one of the conditions you’re monitoring, using a lupus symptom tracker can help you log flares, fatigue, joint pain, and other changes so you can spot patterns and share clearer information with your healthcare provider.
If you notice a mix of these signs, avoid self-diagnosis. Sharing a symptom log with your healthcare provider gives them a clearer picture to work with.
Could one condition make the other worse?
Living with both osteoarthritis and fibromyalgia can sometimes make symptoms feel more intense. One condition doesn’t directly cause the other, but they can influence each other in daily life.
For example, joint pain and stiffness from OA could lead you to move less, which may increase fatigue and discomfort linked to fibromyalgia. Meanwhile, fibromyalgia’s widespread pain, sleep challenges, and fatigue can make OA-related joint pain seem harder to cope with.
Tracking these interactions can help your healthcare provider adjust your plan.
Daily strategies that may help
Managing two chronic conditions can feel overwhelming, but small, steady steps, guided by your healthcare provider - can make daily life more manageable.
{{inline-cta-1}}
Step 1: Track symptoms consistently
Write down or log pain levels, stiffness, sleep, and triggers. Spotting patterns can help you and your doctor understand what’s working.
Try this: The Human Health app makes it easier to track symptoms in one place and share a PDF summary during appointments.
Step 2: Keep moving
Low-impact activities like walking, water exercises, or gentle stretching can help maintain joint flexibility and ease stiffness. Always check with your healthcare provider before making changes to your routine.
Step 3: Focus on rest and stress relief
Relaxation and stress-management techniques, such as progressive muscle relaxation, mindfulness, or gentle breathing exercises, can help people with fibromyalgia become more aware of their bodies, cope better with stress, and reduce pain and tiredness.
Step 4: Follow your agreed-upon care plan
Take prescribed medicines as directed, attend recommended therapy sessions, and keep up with regular check-ins to adjust your plan as needed.
Small steps like these may not erase the challenges, but they can help you feel more organized and supported as you navigate both conditions.
When should you see a doctor?
Reach out to your healthcare provider if you notice new or worsening joint pain, swelling, stiffness, or fatigue, especially if these changes limit your daily activities.
Seek medical attention promptly for sudden swelling, fever, or sharp pain that feels different from your usual symptoms.
Early evaluation helps confirm what’s causing the symptoms and allows your care plan to be adjusted before the situation becomes more challenging to manage.
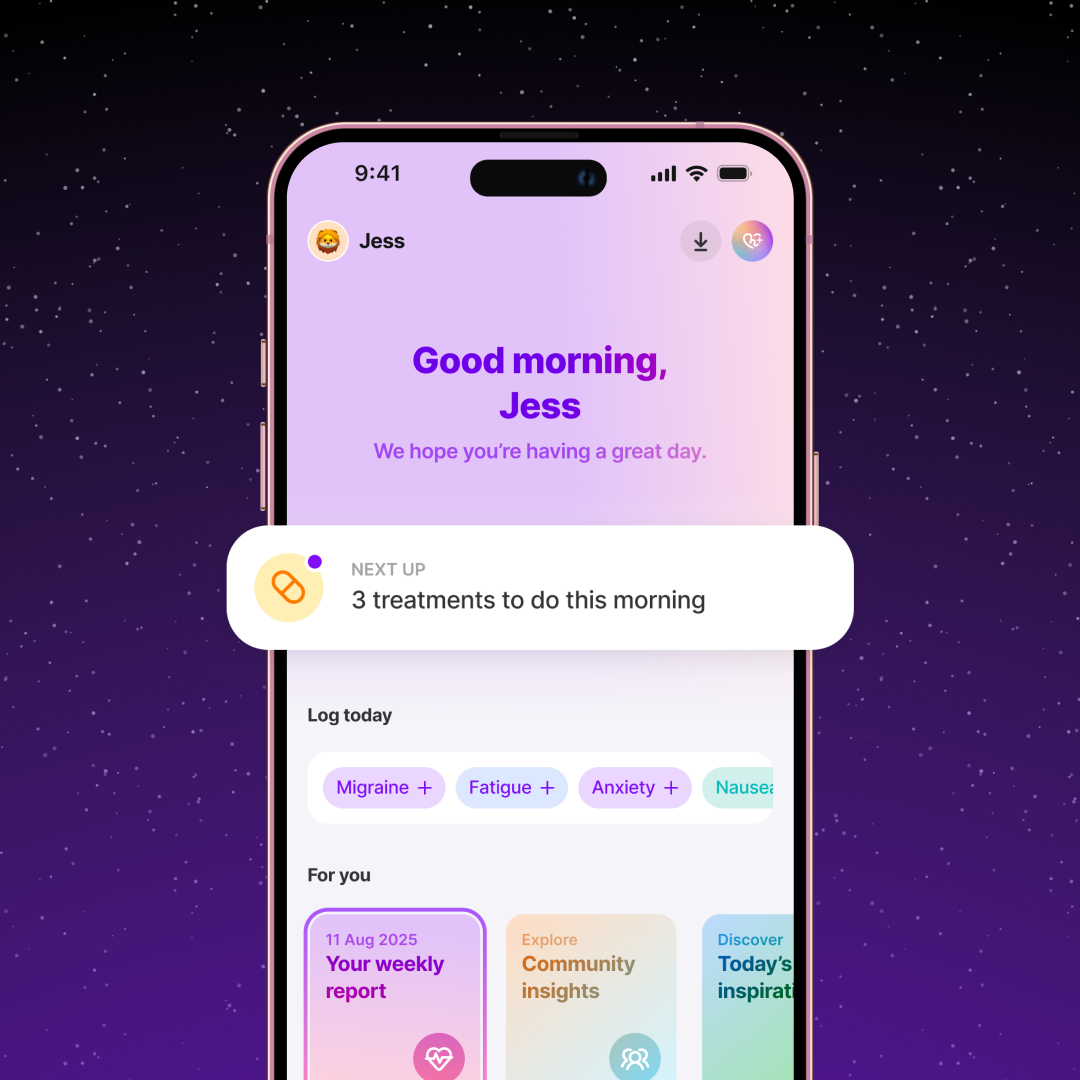
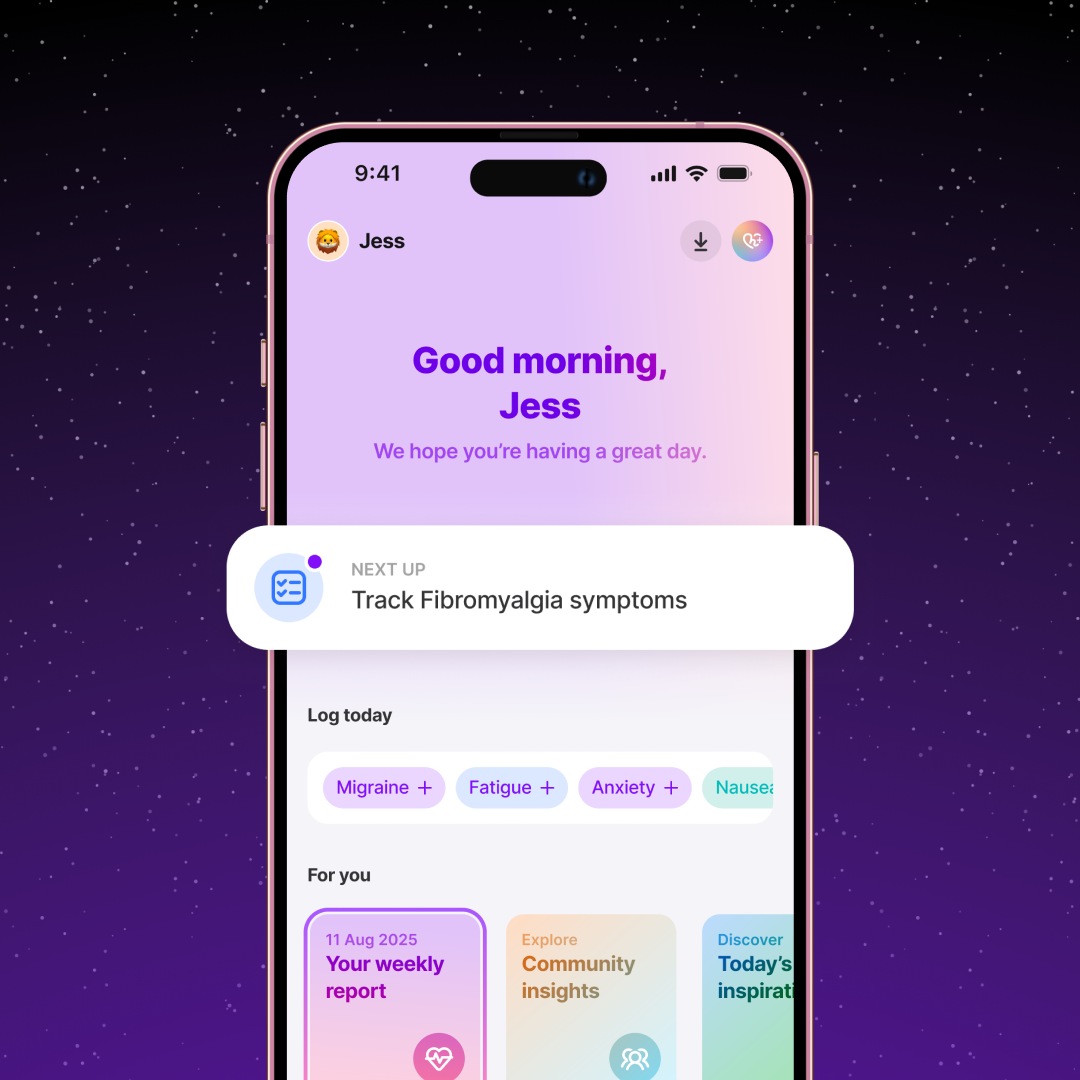
Track osteoarthritis and fibromyalgia symptoms in one place with the Human Health app
Living with two conditions can mean scattered notes, missed details, and appointments where it’s hard to explain everything you’re going through.
The Human Health app brings it together in one place.
You can log pain, stiffness, sleep, and flare-ups, export clear summaries for your healthcare provider, and even manage multiple profiles if you’re also caring for someone else.
The result is fewer loose ends and more confidence that you and your care team are looking at the same picture.
Start today: Track your OA and fibromyalgia symptoms with the Human Health app to feel more prepared and supported in every step of your care.
Disclaimer:
Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- CDC: Osteoarthritis
- National Library of Medicine: Fibromyalgia
- National Library of Medicine: Comorbidity of Fibromyalgia in Primary Knee Osteoarthritis: Potential Impact on Functional Status and Quality of Life
- National Library of Medicine: The Epidemiology and Impact of Pain in Osteoarthritis
- BMC: Perceived function and physical performance are associated with pain and fatigue in women with fibromyalgia
- National Library of Medicine: Impact of fibromyalgia severity on patients mood, sleep quality, and quality of life
- National Library of Medicine: Diagnosis and treatment of hip and knee osteoarthritis: A review
- National Library of Medicine: Neurobiology of fibromyalgia and chronic widespread pain
- Arthritis Foundation: Osteoarthritis: Symptoms, Diagnosis, and Treatment
- Stanford Medicine: Fibromyalgia
- Mayo Clinic: Osteoarthritis - Diagnosis & treatment
- National Library of Medicine: Fibromyalgia: Learn More – Exercise, relaxation and stress management
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

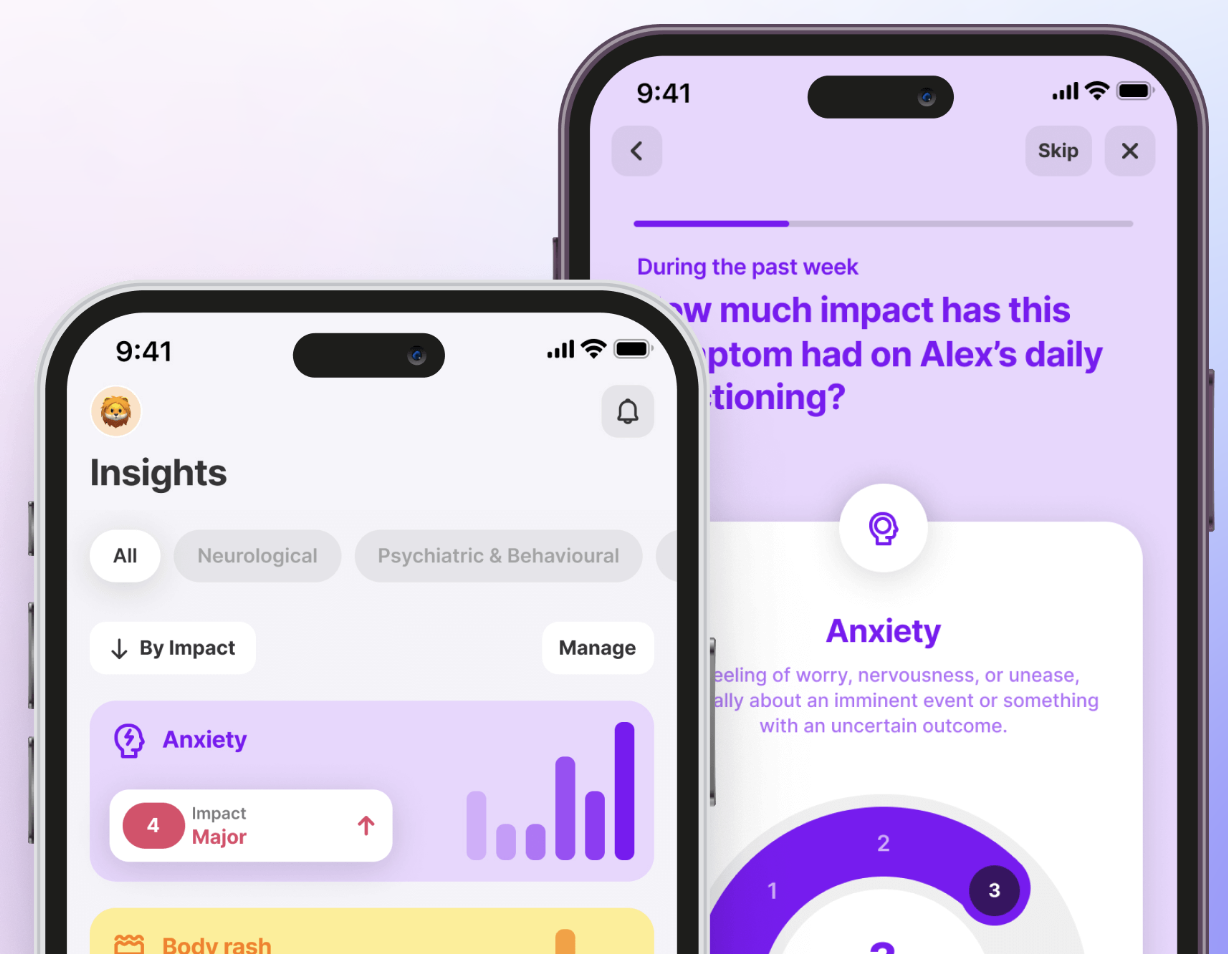
Try The Human Health App For Free!
Add all your symptoms, and track your condition(s) in one place. No more guesswork, or messy notes scattered everywhere. Our app helps you centralize everything.








.jpg)





.png)

