POTS and Pregnancy: Is it Safe? Key Tips & Medication Advice
October 8, 2025

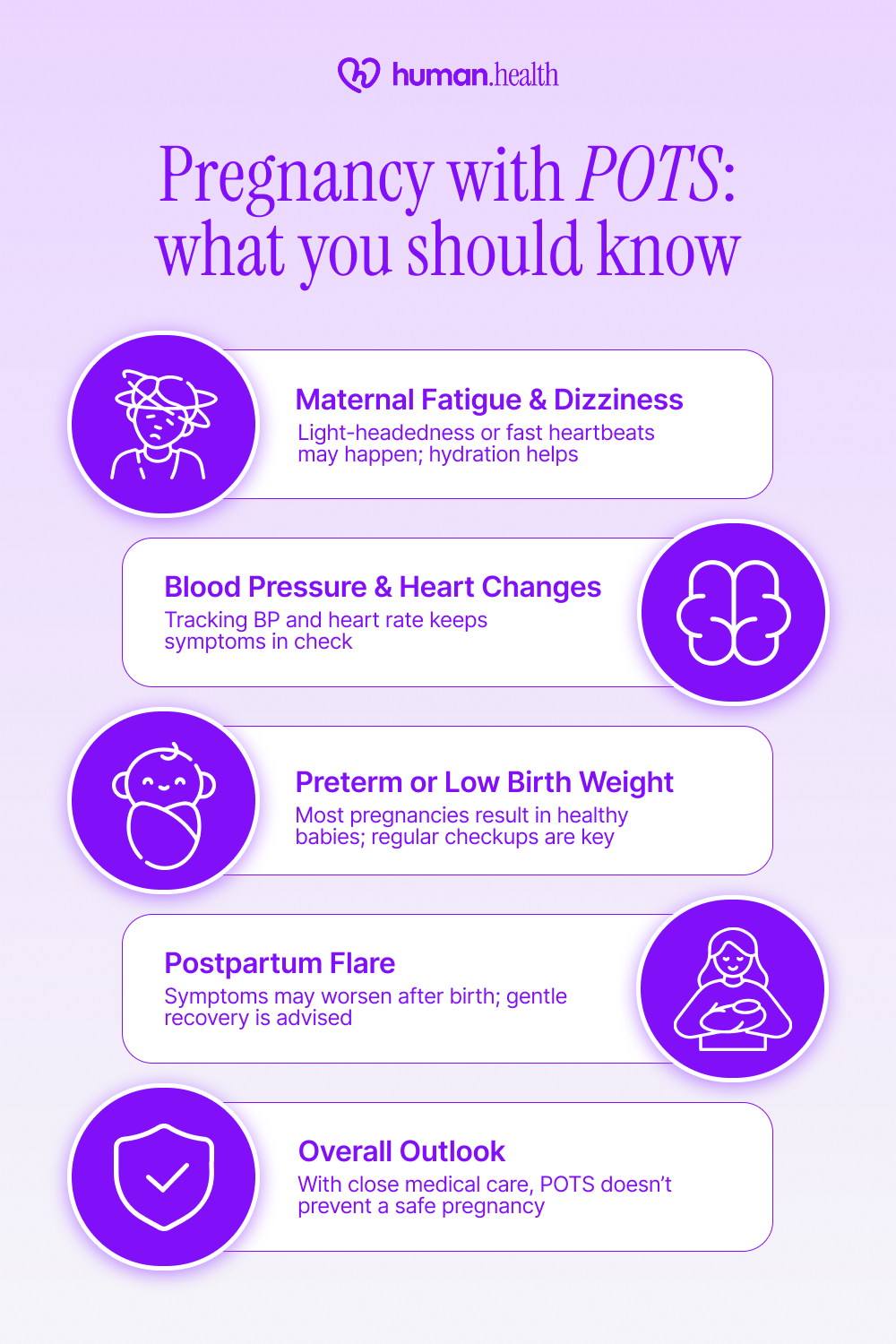
- Pregnancy is generally safe for most people with POTS, though symptoms can change as hormones and blood volume shift. Close monitoring by your healthcare team is important before, during, and after pregnancy.
- Medication safety varies. Some medications, such as beta blockers, may be prescribed under supervision, while others, like stimulants or certain vasoconstrictors, are usually avoided during pregnancy.
- Daily habits can help reduce symptoms, including staying hydrated, increasing salt intake if recommended, and wearing compression garments.
- Tracking your health with the Human Health app allows you to record symptoms, identify triggers, and share insights with your doctor for safer, more personalized pregnancy care.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is for educational purposes only and should not replace consultation with a qualified healthcare provider.
If you’re pregnant and living with postural orthostatic tachycardia syndrome (POTS), it’s natural to have questions. Is it safe? Will your symptoms change? And how can you prepare your body for what’s ahead?
The truth is, many people with POTS go on to have healthy pregnancies. Your body will undergo changes (blood volume increases, heart rate rises, and hormones shift), but with good planning and the right medical support, these changes can be managed safely.
In the next few sections, we’ll look at how pregnancy affects POTS, which medications are generally considered safe, and what lifestyle habits can help you feel more stable day to day. You’ll also discover how the Human Health app can help you track your progress and communicate more easily with your healthcare team.
How may pregnancy affect POTS
Pregnancy brings major changes to the cardiovascular and hormonal systems. Blood volume increases up to 50 %, (with most of that expansion by 34 weeks), heart rate rises by 10–20 bpm, and blood vessels relax to support the growing baby. For people with postural orthostatic tachycardia syndrome (POTS), these shifts can have mixed effects depending on the types of POTS involved.
Some people with POTS experience symptom improvement, particularly in the second and third trimester, likely due to increased blood/plasma volume and hormonal changes. Others may experience worsening orthostatic symptoms (dizziness, fatigue, or heart rate fluctuations), particularly in the first trimester, when the body is still adapting.
Regular monitoring and open communication with your healthcare team are key to managing these changes safely.

Can POTS possibly affect pregnancy outcomes?
A 2009 retrospective study from the University of Toledo followed 22 women with preexisting POTS through their pregnancies. All completed pregnancy successfully, with no stillbirths or major complications, suggesting that many people with POTS can have healthy pregnancies when closely monitored by their healthcare team.
Maternal fatigue and fainting episodes
Some patients report light-headedness or heart rate fluctuations, especially early in pregnancy. Frequent monitoring, hydration, and circulation support may help here.
Blood pressure and heart rhythm changes
Changes in blood pressure or heart rate during pregnancy can make care a little more complex for people with POTS. Tracking these fluctuations helps clinicians manage symptoms and prevent sudden drops that may affect oxygen delivery.
Preterm labor or low birth weight
A 2011 study followed 10 women with POTS through 17 pregnancies, all resulting in live births. Two were preterm, and the rest had normal birth weights, with no birth defects reported. Regular prenatal checkups and early communication about symptoms were linked to better outcomes.
Postpartum symptom flare
In one study, up to 31% of people with POTS experienced symptom worsening postpartum, likely due to rapid hormonal and blood volume shifts. Gradual recovery and gentle pacing are often advised under medical guidance.
With consistent medical care and early planning, people with POTS can have safe pregnancies and recover well.
Can you take POTS medications during your pregnancy?
Medication decisions during pregnancy always require medical supervision. For people with postural orthostatic tachycardia syndrome (POTS), the safety of continuing or stopping medication depends on the drug type, dosage, and how symptoms affect daily function.
What medications are considered safer
In hypertensive pregnancies, labetalol is commonly used to manage blood pressure and may help reduce the incidence of severe hypertension.
In some cases, low-dose fludrocortisone or midodrine may be continued during pregnancy, though this requires close oversight from both obstetric and cardiology specialists, given limited safety data.
What medications to avoid taking during pregnancy
Central nervous system (CNS) stimulants (e.g., amphetamines, methylphenidate) are generally avoided in pregnancy because exposure has been associated with increased risk of congenital anomalies, fetal growth disturbances, or neonatal morbidity. Always consult your provider before changing or stopping any medication.
{{pro-tip-1}}
A medication review early in pregnancy helps you and your provider find the safest balance between symptom relief and the baby’s well-being.

Managing postural orthostatic tachycardia syndrome (POTS) during pregnancy focuses on lifestyle habits that help stabilize blood flow and energy. In addition to medical guidance, exploring natural remedies for POTS can offer supportive strategies for managing symptoms safely. Because each person’s response is unique, these adjustments should always be guided by your healthcare provider.
Stay hydrated and maintain electrolyte balance
Drinking enough fluids supports blood volume and may help reduce dizziness or fainting episodes. In fact, guidance for POTS includes increasing fluid intake to at least 2.5 L per day. Tracking hydration levels daily can help you notice patterns and adjust more consistently.
Adjust salt intake if advised
Moderately increased salt intake can help the body retain fluid and support stable blood pressure in POTS, but this should only be done under medical supervision. Recording salt intake and symptoms in the Human Health app can reveal how your body responds over time.

Wear compression garments
Compression stockings or maternity-friendly garments (e.g., waist-high stockings) can reduce venous pooling in the legs and improve circulation. Wearing them during long periods of standing or travel may help some people feel less dizzy or fatigued.
Focus on gentle movement and pacing
Graded, light activity (such as walking or gentle prenatal yoga) may support circulation and help prevent deconditioning in POTS. Balancing rest and movement helps manage fatigue without overexertion.
Use the Human Health app to log daily symptoms, monitor triggers, and share patterns with your doctor. Tracking over time can make it easier to see what strategies work best for you and when adjustments are needed.
Labor and delivery: special considerations for POTS patients
Labor and delivery are generally safe for people with postural orthostatic tachycardia syndrome (POTS), but special planning helps ensure stability and comfort. Communicate early with your obstetric and anesthesia teams about your diagnosis and any triggers or sensitivities.
Monitoring heart rate and blood pressure
Continuous monitoring during labor helps manage sudden changes in blood pressure or heart rate, which can occur due to positioning or pain responses. Careful observation allows your medical team to respond quickly if symptoms arise.
{{inline-cta-1}}
Pain management options
For people with POTS, epidural anesthesia is generally considered safe during labor and may help reduce heart rate spikes caused by pain. When used, it is typically given slowly and after fluids are provided to lower the chance of low blood pressure. Talk with your anesthesiologist ahead of time about what approach will work best for you.
Positioning and hydration
During labor, staying in a semi-reclined or side-lying position (such as the left side) may help improve blood flow back to the heart and reduce pressure on major veins. Intravenous fluids may be used when needed to help maintain blood pressure and circulation. Planning these supports in advance with your care team can promote stability throughout delivery.
Postpartum care
After childbirth, changes in blood volume and increased fluid loss can temporarily make POTS symptoms feel worse. Taking things slowly, staying hydrated, and following supportive care can help your body recover. Having a postpartum plan in place with your care team makes it easier to manage flares and protect your well-being.
With thoughtful preparation and communication between you and your care team, labor and delivery can be managed safely and confidently for people with POTS.
Can POTS be inherited by your baby?
POTS doesn’t appear to follow a simple inherited pattern, but family history can play a role. In one study, around 14% of people with POTS had a family member with the condition, and about 31% had a relative with orthostatic intolerance, suggesting a possible genetic tendency, though the exact cause is still unknown.
Environmental or physical stressors such as viral infections, hormonal changes, or puberty may trigger symptoms in people who are already genetically predisposed. If POTS runs in your family, letting your child’s doctor know can support early awareness and monitoring. Genetics may increase the likelihood, but it doesn’t mean your baby will develop POTS.
There’s currently no evidence that having POTS affects a baby’s development, but keeping your healthcare team informed helps ensure proactive care if symptoms ever arise.
Track POTS symptoms and changes inside the Human Health app
Managing POTS during pregnancy often means adjusting as you go. Tracking what helps, what worsens symptoms, and how your body changes each trimester can make a real difference in how you feel and how confident you are.
With the Human Health app, you can log symptoms like dizziness, fatigue, or rapid heart rate, keep track of hydration and nutrition, and note any treatments or lifestyle changes your doctor recommends. You can also create a clear, shareable summary for prenatal or cardiology visits, so your care team can easily spot patterns and tailor your care.
Consistent tracking helps you and your providers understand your body better and make informed, safer decisions throughout pregnancy and recovery.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- National Library of Medicine: Physiological changes in pregnancy
- National Library of Medicine: POTS and Pregnancy: A Review of Literature and Recommendations for Evaluation and Treatment
- National Library of Medicine: Symptoms of postural orthostatic tachycardia syndrome in pregnancy: a cross-sectional, community-based survey
- National Library of Medicine: Effect of Pregnancy on Postural Tachycardia Syndrome
- Dysautonomia Youth Network of America: Outcomes of Pregnancy in Patients with Preexisting Postural Tachycardia Syndrome
- ResearchGate: Pregnancy in postural tachycardia syndrome: clinical course and maternal and fetal outcomes
- ScienceDirect: Oral antihypertensive treatment during pregnancy: a systematic review and network meta-analysis
- Standing Up to POTS: Pregnancy in POTS Patients
- National Library of Medicine: The Use of Central Nervous System Active Drugs During Pregnancy
- Cleveland Clinic Journal of Medicine: Evaluating and managing postural tachycardia syndrome
- Autonomic Neuroscience: Basic and Clinical: Overview of the management of postural tachycardia syndrome in pregnant patients
- National Library of Medicine: Exercise Interventions in the Management of Postural Orthostatic Tachycardia Syndrome: A Scoping Review
- ResearchGate: Anaesthetic management of a parturient with the postural orthostatic tachycardia syndrome: A case report
- Autonomic Neuroscience: Basic and Clinical: Overview of the management of postural tachycardia syndrome in pregnant patients
- National Library of Medicine: Postural orthostatic tachycardia syndrome (POTS): State of the science and clinical care from a 2019 National Institutes of Health Expert Consensus Meeting - Part 1
- Cambridge Core: Family history of associated disorders in patients with postural tachycardia syndrome
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Track Your Health Daily
Record your symptoms and notes, set reminders, and monitor your treatments easily with the Human Health app.







Pro tip
Keep a medication log before, during, and after pregnancy.
Recording dose changes, start and stop dates, and how often you take your treatments could help your doctors coordinate care and make safer adjustments.
Learn more about tracking your treatments for better communication with your healthcare team.

.jpg)




.png)

