Is POTS Genetic? Key Insights, Studies & Data
October 4, 2025

- Research has not yet proven a strong link between certain genes and POTS.
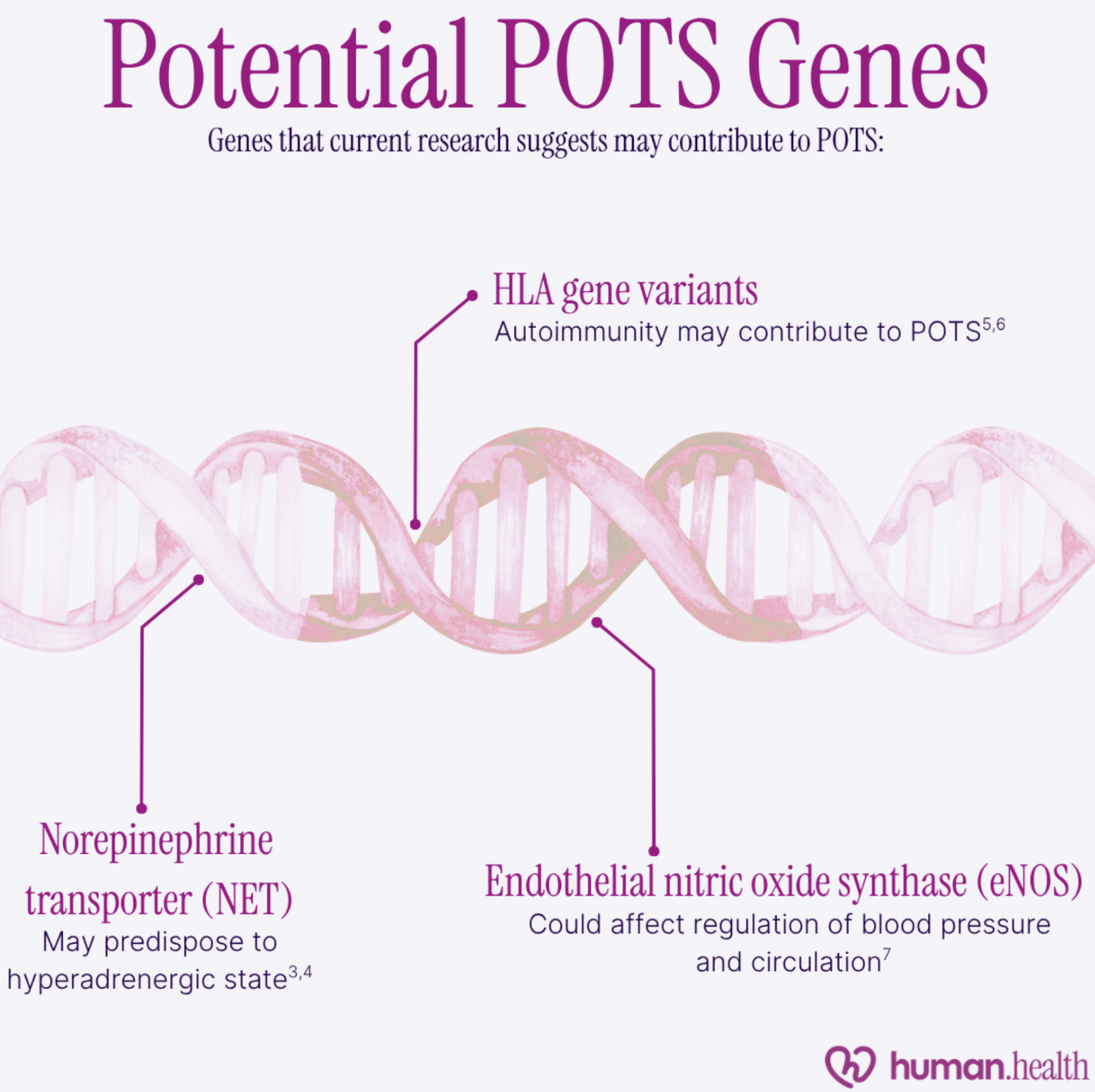
- Variations in some genes, such as the norepinephrine transporter (NET), human leukocyte antigen (HLA), and endothelial nitric oxide synthase (eNOS), are being studied for their involvement in POTS.
- Other genetic conditions, such as autoimmunity, connective tissue diseases, diabetes mellitus, and familial dysautonomia, may contribute to increased risk of POTS.
- Using a health-tracking app like Human Health may help you identify patterns in your POTS symptoms, so you can understand what’s triggering them.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor or healthcare provider before making changes to your health routine or starting any new treatment.
Many chronic conditions are heritable through our genes, but is POTS one of them?
POTS, short for postural orthostatic tachycardia syndrome, affects blood pressure and circulation. Medical literature has described patients with POTS-like symptoms since the 1800s, yet researchers have not identified exactly why the condition develops.
Recent advances in research have highlighted some potential genes that could help us understand POTS. In this article, we’ll explain the role genes play in the development of chronic conditions, which genes and risk factors could be involved in POTS, and how these could influence the symptoms and management of this complex condition.
What current research suggests about the genetics of POTS
As is true for many chronic conditions, it’s likely that the onset of POTS is multifactorial. Gene variations, autoimmunity, viral illnesses, psychological stress, anatomical variations, and hormonal changes are just some of the pathways that have been implicated as potential contributors towards the development of POTS.
Although a clear genetic cause for POTS has not yet been defined, research in this area is evolving, and new evidence has suggested a couple of potential genetic targets that may be linked to the condition.
Genetic vs inherited: What’s the difference?
We don’t yet know if POTS is a genetic condition, or if it can be inherited. These terms are often used interchangeably, but there’s an important distinction between them.
A genetic condition is any condition that arises due to changes in our DNA, whether these changes were passed down to us from our family or occur spontaneously in an individual.
Inherited conditions are passed down between relatives. At least one parent must carry a copy of the gene variant associated with the condition, and sometimes the condition only develops if both parents are carriers. Examples include cystic fibrosis, sickle cell anemia, and Huntington's disease.
You can also explore a detailed comparison of POTS and anemia in our in-depth guide.
In short, all inherited conditions are genetic, but not all genetic conditions are inherited.

Genes that might be associated with POTS
To our current knowledge, there isn’t a direct genetic cause for POTS. However, some smaller studies have produced evidence leading to an emerging understanding that some genetic variants may contribute to an increased risk of POTS.
Norepinephrine transporter (NET)
Hyperadrenergic POTS is a subtype in which patients have higher than typical levels of a chemical called norepinephrine (or noradrenaline) in the body. Norepinephrine is released when the brain senses a threat to the body, such as low blood pressure. This is commonly known as the ‘fight or flight’ response.
A case-based study from 2000 centered around a family with a high incidence of POTS-like symptoms found variation in the norepinephrine transporter gene (NET), also known as SLC6A2. NET is a protein responsible for recycling norepinephrine so there isn’t too much of it active for too long. However, in this family, affected individuals had a 98% loss of function in NET compared to those unaffected.
It’s important to note that the main focus of this study were two identical twin sisters with this gene variation and POTS-like symptoms, along with anatomical changes to the heart. Some other family members carried the same gene variation, but did not have the anatomical changes or symptoms as severe as the twins.
This further emphasizes that even with a strongly associated genetic component, development of POTS symptoms may be also dependent on other factors.
Other researchers have identified that medications which inhibit NET can induce orthostatic tachycardia (atypical increase in heart rate with standing), adding more weight to the evidence from the case study. Research into the role of NET in POTS is ongoing to confirm its role in the condition.
{{inline-cta-1}}
HLA genotypes and autoimmunity
Short for human leukocyte antigen, the HLA gene codes for a protein that sits on the surface of most of our cells, and helps our immune system differentiate between self and non-self cells.
A Korean study of 17 patients diagnosed with POTS identified that 41% had the DQB1*06:09 variant of HLA, compared to only 7% of the control group, suggesting a potential link between this genotype and POTS risk.
For some people, the HLA system doesn’t work properly, and that can lead to an autoimmune disease, where the immune system mistakenly attacks the body’s own cells.
An abstract published in the renowned scientific journal Neurology in 2021 found that within a group of 93 participants in the U.S., HLA variations previously associated with autoimmune conditions were found to occur at high frequency in POTS patients. This included variants HLA-B*15:01, B*40:01, DQB*1*02:01,and DRB1*03:01.
More studies demonstrating an association between these particular HLA groups and POTS are required to solidify the link between HLA variants and POTS risk.
Endothelial Nitric Oxide Synthase
Nitric oxide is a chemical that acts in various ways on the cardiovascular system to regulate blood pressure and circulation. It is produced by a protein called endothelial nitric oxide synthase (eNOS) in the endothelial cells, which line the blood vessels.
A 2005 observational study of 136 POTS patients in both the U.S. and Austria identified variation in the gene coding for eNOS, which could affect the production of nitric oxide and subsequently alter the regulation of blood pressure and circulation, as is seen in POTS. Additional research is required to confirm the association.
Related heritable conditions that may raise POTS risk
There are some other conditions that are known to have a genetic component to their development, which may be associated with increased risk of POTS. Having any of these conditions does not guarantee affected individuals will also develop POTS.
Connective tissue diseases
A 2018 literature review identified that between 20–50% of patients with POTS are also diagnosed with Ehlers-Danlos syndrome (EDS), a condition that affects the integrity of connective tissues in the body.
Blood vessels are made of connective tissue, and therefore their function in regulating blood pressure could be influenced by the structural changes seen in EDS, which may help explain how POTS and EDS are related.
Many forms of EDS are linked to heritable variations in genes that code for connective tissue proteins, like collagen and tenascin.
Autoimmune conditions
Through surveys and retrospective data analyses conducted in the U.S., U.K., and
Canada, researchers found that up to 20% of POTS patients also had another autoimmune disease. This included but was not limited to systemic lupus erythematosus, Sjögren’s syndrome, Celiac disease, and thyroid disease.
If you’re living with both POTS and lupus, using a tool to track lupus symptoms can help you keep a clear record of flares, fatigue, and pain so you can see how they might interact with your POTS symptoms over time.
As mentioned above, when the immune system malfunctions and attacks the body’s own cells, it can leading to inflammation and damage, which causes various symptoms of disease.
Although the onset of autoimmune diseases can be multifactorial, genetic factors such as specific HLA variants are known to increase risk for developing the disease.
You can also explore more about Is POTS an Autoimmune Disease to better understand how POTS may relate to immune system dysfunction.
Diabetes mellitus
Diabetes is a condition that arises as a result of dysregulation of sugar (glucose) concentration in the blood. High blood glucose can cause damage to nerves, heart cells, and blood vessels, which can affect the regulation of blood pressure.
Some people with diabetes develop POTS as a secondary condition as a result of these complications.
You can learn more about how these two conditions are connected in our detailed guide on POTS and blood sugar.
Familial dysautonomia
Some people inherit a specific variant in the gene that codes for Elongator complex protein 1 (ELP1). ELP1 is crucial for the development and survival of nerves. People with this condition are affected from birth by complications such as gastrointestinal dysfunction, seizures, recurrent lung infections, and more. Of interest is the related autonomic dysfunction which can lead to both hypotensive and hypertensive crises, which may present with POTS-like symptoms.
Learn more about the connection between POTS and seizures, and how autonomic dysfunction influences these conditions.
How genetics may influence POTS
We’ve already established that POTS development is multifactorial, with genetics potentially contributing to the condition. There are some ways that genetics could influence POTS presentations and management.
Onset of symptoms
For many genetic conditions, onset of the disease occurs earlier in life than for conditions which are acquired or develop later in life, independent of genetic predisposition.
Theoretically, this may mean that people with genetic variants associated with POTS may experience an earlier onset of symptoms, compared to individuals who don’t have these variants.
Research on the timing of onset for POTS symptoms in patients with genetic variants of interest has not yet been established.
Persistence of disease
We’re born with our genes, and although research in gene therapy is advancing, we might still be a long way from accessibility to treatments which can override our genetics and replace or fix gene variants that cause disease.
Although this has not yet been backed up by clinical research, it’s possible that people with POTS-associated genes may experience larger difficulty maintaining control over their symptoms. Because of the fixed nature of our genes, gene variation may produce persistent autonomic dysfunction despite intervention.
Potential treatment targets
Advancements in genetic research have created new opportunities for developing treatments that treat the root cause of genetic conditions.
If further research confirms strong associations between certain genes and POTS, it’s possible that more treatment options will become available for the condition.
For example, medications that increase activity of the norepinephrine transporter or endothelial nitric oxide synthase proteins could be potential targets for research.
Identifying if autoimmunity contributes to POTS could indicate utility for immunological therapies to reduce aberrant immune responses contributing to POTS.
Managing POTS with genetics in mind
There are strategies to manage POTS symptoms, regardless of whether genetics has contributed to development of these symptoms or not.
Awareness of overlapping conditions
Being aware of which conditions could be associated with POTS may help you structure appointments with your healthcare team, who can help advise you about what to lookout for.
For instance, understanding the link between MCAS and POTS can provide deeper insight into how these conditions may overlap and influence each other’s symptoms.
{{pro-tip-1}}
Optimize lifestyle factors
You can’t change your genes, but you can change your lifestyle. Particularly for POTS, changes like increasing water and salt intake, frequent aerobic exercise, decreasing time spent lying down, and maintaining a good sleep schedule are recommended by experts to manage the condition.
Staying consistent with these strategies to try and control your symptoms may give you the best chance at overcoming the effects of any gene variants playing a part in your POTS.
Adjusting your treatment plan
Work with your healthcare team to ensure that your treatment plan is tailored to your symptoms and needs, such as counteracting the effects of any genetic variants you may have that could contribute to POTS.
Not sure how to be sure if your treatments are working for you? The Human Health app can help you track the impact of your symptoms as they happen, to show you and your treating team how well they’re being managed.
Should you get genetic testing for POTS?
As of 2025, further research is still required to provide robust evidence for which gene variations are associated with POTS, and because of this limitation, genetic testing specifically for POTS may not be available.
Your doctor will be able to give you information about what genetic tests may be available for you and if you should have them.
Even if research suggests that some genes are associated with the condition, the diagnostic criteria for POTS is still based on clinical signs and symptoms, not the presence of genetic markers.
How the Human Health app can help you track your POTS symptoms
The Human Health app is a mobile tool created for people with chronic conditions like POTS. Managing complex conditions alone can be daunting, and Human is designed to be your helping hand in keeping track of how your health is changing. With all the information that matters to you in one place, Human can make advocating for your health easier.
Some of the features of the Human Health app that could benefit people with POTS include:
- Daily symptom tracking, with comprehensive Insights so you and your doctor can visualize how symptoms, like dizziness and headache, are really impacting you day-to-day
- Downloadable reports you can share with your healthcare team and loved ones, so they can see a clear and concise summary of your health journey
- Record test results such as blood pressure readings, electrolyte levels and more
- Treatment Plan keeps an accurate record of treatments you’re taking or have taken in the past, so you don’t have to remember off the top of your head
- Brain fog affecting your memory? Get reminder notifications when a treatment is due, or an appointment is coming up
Say goodbye to the pressure of POTS management. Get started for free with the Human Health app today.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- Klaas, K., Kavi, L. (2021). Historical Background. In: Gall, N., Kavi, L., Lobo, M.D. (eds) Postural Tachycardia Syndrome. Springer, Cham. https://doi.org/10.1007/978-3-030-54165-1_2
- Zhao S, Tran VH. Postural Orthostatic Tachycardia Syndrome. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541074/
- Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D. Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med. 2000 Feb 24;342(8):541-9. doi: 10.1056/NEJM200002243420803. PMID: 10684912.
- Raj SR. The Postural Tachycardia Syndrome (POTS): pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006 Apr 1;6(2):84-99. PMID: 16943900; PMCID: PMC1501099.
- Shin YW, Moon J, Kim TJ, Kim DY, Chang H, Jun JS, Lee ST, Jung KH, Park KI, Jung KY, Kim M, Lee SK, Chu K. Human leukocyte antigen associations in postural tachycardia syndrome. Ann Clin Transl Neurol. 2019 Apr 4;6(5):962-967. doi: 10.1002/acn3.766. PMID: 31139694; PMCID: PMC6529927.
- Orban Z, Miller A, Bourne K, Nitis J, Hu W, Reinsel H, Stiles L, Fedorowski A, Axelsson J. Immunogenetic Risk Markers in Postural Orthostatic Tachycardia Syndrome (4709). Neurology 2021; 96(15_Supp). https://www.neurology.org/doi/10.1212/WNL.96.15_supplement.4709
- Garland, E. M., Winker, R., Williams, S. M., Jiang, L., Stanton, K., Byrne, D. W., ... & Robertson, D. (2005). Endothelial NO synthase polymorphisms and postural tachycardia syndrome. Hypertension, 46(5), 1103-1110.
- Fedorowski, A. (2019). Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. Journal of internal medicine, 285(4), 352-366.
- Miklovic T, Sieg VC. Ehlers-Danlos Syndrome. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549814/
- Vernino, S., & Stiles, L. E. (2018). Autoimmunity in postural orthostatic tachycardia syndrome: current understanding. Autonomic Neuroscience, 215, 78-82.
- Glasgow, A. C., & Kim, J. Y. (2024). Metabolic targets in the Postural Orthostatic Tachycardia Syndrome: A short thematic review. Autonomic Neuroscience, 103232.
- OMIM (Online Mendelian Inheritance in Man). #223900. Neuropathy, Hereditary Sensory And Autonomic, Type III; HSAN3. Available at: https://omim.org/entry/223900
- UpToDate. Postural tachycardia syndrome. Available at: https://www.uptodate.com/contents/postural-tachycardia-syndrome
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Track Your POTS Symptoms In Our App!
With the Human Health app - you can track your POTS symptoms, add notes, reminders, and so much more! Try it today, for free.







Pro tip
Using a health tracking app like Human Health could be useful to keep a log of any new symptoms you experience, to follow-up with your treating team at your next appointment.

.jpg)




.png)

