Is POTS an Autoimmune Disease? What Studies Say [2025]
November 26, 2025

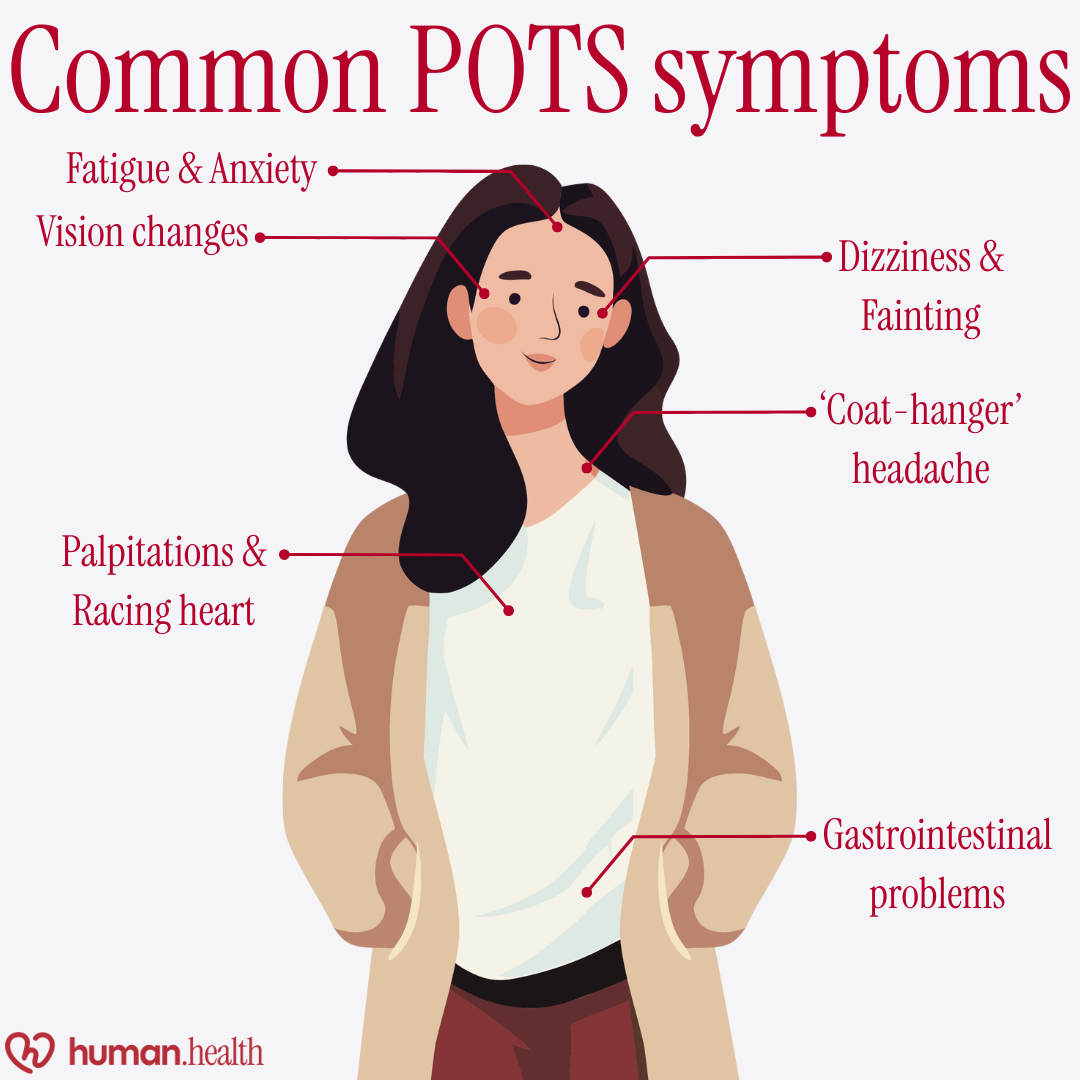
- Postural orthostatic tachycardia syndrome (POTS) happens when your heart rate rises sharply after standing, causing dizziness, fatigue, or lightheadedness.
- Studies suggest that some people with POTS will also have autoimmune conditions such as celiac disease, thyroid disorders, or Sjögren’s syndrome. However, this connection is still being studied.
- POTS may develop after infections, hormonal changes, or periods of illness such as long COVID.
- There is no cure, but symptoms can often be managed with the help of increased fluids and salt, compression wear, and gradual physical activity under medical guidance.
Disclaimer: This article is for informational purposes only and should not be taken as medical advice. Always speak with a qualified healthcare provider about your symptoms or treatment options.
If standing up makes your heart race, your head spin, or your body feel drained, you’re not alone. Many people living with postural orthostatic tachycardia syndrome (POTS) experience these feelings daily.
Scientists are still studying whether POTS is an autoimmune disease. So far, research shows possible links with autoimmune activity, but no clear proof that it directly causes the condition.
In this article, you’ll learn what the latest studies reveal, which autoimmune disorders are often seen alongside POTS, and how to manage symptoms more confidently.
What is postural orthostatic tachycardia syndrome (POTS)?
Postural orthostatic tachycardia syndrome, or POTS, is a disorder of the autonomic nervous system that affects how your body controls blood flow and heart rate. When someone with POTS stands up, their heart rate rises sharply (usually by at least 30 beats per minute within ten minutes of standing) without a drop in blood pressure. This sudden change can cause dizziness, lightheadedness, or fainting.

POTS is not a heart disease or an anxiety disorder; it is a form of dysautonomia, meaning it stems from the part of the nervous system that manages automatic body functions like heartbeat, breathing, and digestion. The condition mainly affects women between adolescence and middle adulthood, and studies suggest it may occur in up to one percent of the population.
Autoimmune disease connection to POTS: What the studies say
Researchers are still studying whether POTS may have an autoimmune element. Evidence shows that some people with POTS also have an autoimmune disorder. A recent review found that, overall, autoimmune diseases were more common in POTS patients, with pooled ratios suggesting about two and a half times the usual rate. Celiac disease, in particular, appeared roughly 2.7 times more frequently.
Ehlers-Danlos syndrome, although not autoimmune, is another condition often seen in people with POTS. It affects connective tissue and can contribute to symptoms like dizziness and fatigue. Because these overlaps vary from person to person, doctors often check for signs of autoimmune activity when diagnosing and managing POTS.
Other immune conditions, such as Hashimoto’s disease, lupus, and Sjögren’s syndrome, have also been reported in smaller studies.
Current evidence, therefore, supports a possible autoimmune connection but not firm proof that POTS itself is an autoimmune disease.
What may be causing POTS
The exact cause of POTS isn’t clear. Research indicates that several body systems may be involved, and individuals can develop POTS for various reasons.
Current theories behind why POTS develops
Scientists describe three main ideas about how POTS develops.
- One involves the immune system, which may sometimes affect the nerves that control blood flow.
- Another theory suggests the body’s “fight or flight” system becomes overactive, leading to a rapid heart rate when standing.
- The final theory points to nerve dysfunction that causes poor circulation and low blood volume, so the heart beats faster to compensate.
These theories may overlap, which is why POTS can be experienced differently from person to person.
Triggers and risk factors
Certain factors may increase the chance of developing POTS or make symptoms worse. Reported triggers include viral infections, physical trauma, or surgery, and changes in hormones, such as during puberty or pregnancy. People are also more likely to develop POTS if they have long COVID, chronic fatigue syndrome, or joint hypermobility.
Learn about the different types of POTS and their impact.
The everyday impact of POTS symptoms
People with POTS may feel light-headed, dizzy, or faint shortly after standing. The heart may race, sometimes causing chest pain, shaking, or shortness of breath. Other common complaints include fatigue, weakness, and brain fog, meaning trouble with memory or focus. Symptoms may vary from day to day and can be worse in the morning.
These recurring issues can make daily life challenging. Tasks that involve standing, concentration, or sustained effort may become difficult, while fatigue and dizziness can limit work, school, and social activities.
For additional context on how POTS can affect daily activities, see our in-depth guide on driving with POTS syndrome.
See what happens during a POTS episode.
{{pro-tip-1}}
Managing POTS
There is currently no cure for POTS, but symptoms can often be managed through lifestyle adjustments and medical guidance. Tools like the Human Health app can make this process easier by helping you track symptoms and lifestyle changes over time.
{{inline-cta-1}}
Lifestyle adjustments
Doctors usually begin with lifestyle approaches such as increasing daily fluid and salt intake, eating smaller meals lower in refined carbohydrates, and wearing compression garments to improve blood flow.
Exercise or rehabilitation programs are also recommended for people with dysautonomias like POTS, to build stamina and support the body’s natural regulation of blood flow. These are introduced gradually, often under supervision.
{{pro-tip-2}}
Medications and treatments
If lifestyle adjustments are not enough, medicines may be prescribed to help control heart rate and blood pressure. Emerging evidence suggests other therapies are being studied, including ivabradine and intravenous immunoglobulin, though these remain experimental and require more research.
Because responses vary, treatment plans are individualized, combining several of these measures under specialist supervision, with adjustments as symptoms change.
Finding the right combination of strategies can take time, but with consistent care, people learn to manage their symptoms and regain a more stable daily routine.
Managing POTS: How Human Health can help
Managing POTS takes patience, consistency, and the right support. While there’s no single solution, tracking symptoms and spotting patterns can make a real difference.
The Human Health app allows you to log daily experiences, including heart rate, fatigue, and hydration levels, providing a clearer picture of what triggers your symptoms.
By combining data insights with guidance from your healthcare provider, you can adjust your routine more effectively, whether that means pacing physical activities, increasing fluids, or fine-tuning sleep and nutrition.
Take the next step toward understanding your body better. With the Human Health app, you can track symptoms, spot patterns, and feel more confident managing POTS day by day.
References
- Raj SR, Fedorowski A, Sheldon RS. Diagnosis and management of postural orthostatic tachycardia syndrome. Canadian Medical Association Journal. 2022;194(10):E378–E385. doi:https://doi.org/10.1503/cmaj.211373
- NHS. Postural tachycardia syndrome (PoTS). NHS. Published 2023. https://www.nhs.uk/conditions/postural-tachycardia-syndrome/
- Aboseif A, J. Daniel Bireley, Li Y, Polston D, Abbatemarco JR. Autoimmunity and postural orthostatic tachycardia syndrome: Implications in diagnosis and management. Cleveland Clinic Journal of Medicine. 2023;90(7):439–447. doi:https://doi.org/10.3949/ccjm.90a.22093
- Sebastian SA, Co EL, Panthangi V, et al. Postural Orthostatic Tachycardia Syndrome (POTS): An Update for Clinical Practice. Current Problems in Cardiology. 2022;47(12):101384. doi:https://doi.org/10.1016/j.cpcardiol.2022.101384
- Mannan H, Pain CM. Sex adjusted standardized prevalence ratios for celiac disease and other autoimmune diseases in patients with postural orthostatic tachycardia syndrome (POTS): A systematic review and meta-analysis. Heliyon. 2023;9(2):e12982. doi:https://doi.org/10.1016/j.heliyon.2023.e12982
- Treadwell JR, Wagner J, Reston JT, Phillips T, Hedden-Gross A, Tipton KN. Treatments for Long COVID autonomic dysfunction: a scoping review. Clinical autonomic research: official journal of the Clinical Autonomic Research Society. 2025;35(1):5–29. doi:https://doi.org/10.1007/s10286-024-01081-w
Disclaimer: This article is for general informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional before making decisions about diagnosis or treatment.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Track your POTS symptoms with the Human Health app
Record daily symptoms like dizziness, fatigue, or rapid heartbeat to spot patterns and better understand your body’s responses.







Pro tip
Try noting when your symptoms are worst: morning, after meals, or during hot weather. Recognizing patterns can help your doctor personalize treatment and identify triggers faster.
Pro tip
If you’re starting an exercise program or salt-loading plan, increase gradually and keep a simple daily log. Even small changes can make a difference. Using the Human Health app to track your salt, fluids, and fatigue helps you see which adjustments actually work for you.

.jpg)




.png)

