Types Of POTS: Management Advice & More
September 24, 2025

- POTS subtypes include neuropathic, hypovolemic, hyperadrenergic, and cardiovascular deconditioning.
- POTS can be primary (occur in isolation), or secondary to another condition, such as autoimmune conditions, viral infections, diabetes, or hypermobility disorders.
- Common POTS symptoms include dizziness, fainting, fatigue, anxiety, vision changes, headache, and gastrointestinal problems. Seek medical attention if symptoms are a cause of concern.
- To manage POTS, experts recommend maintaining fluid and electrolyte balance, aerobic exercise, good sleep hygiene, and compression garments.
- The Human Health app can help people with POTS manage their health, with features such as symptom and treatment trackers, appointment reminders, downloadable reports, and more.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor or healthcare provider before making changes to your health routine or starting any new treatment.
POTS is a complex chronic condition, and its presentations can be classified in various ways, which can be confusing if you’re trying to learn about the condition for the first time.
In this post, we’ll explore the suggested subtypes of POTS, other conditions that might lead to POTS, and how to manage it.
What is POTS?
Short for postural orthostatic tachycardia syndrome, POTS is a condition that affects how the body adjusts blood pressure to changes in position. Blood can pool in the lower body when you’re sitting or lying down, and when you stand up, it usually gets pumped back to the upper body so that important organs like the heart and brain get enough oxygen.
For people with POTS, this process doesn’t work properly, and they can experience symptoms like a racing heart, dizziness, and fainting as a result. This phenomenon is known as orthostatic intolerance.
The different types of POTS
There are a couple of ways POTS can be divided into subtypes. An international expert consortium created a consensus document which outlined subtypes based on some physical mechanisms that may lead to POTS symptoms. These may overlap, and the distinction may not be clear for each patient. There may also be more unknown mechanisms that could play a part in development of the condition.
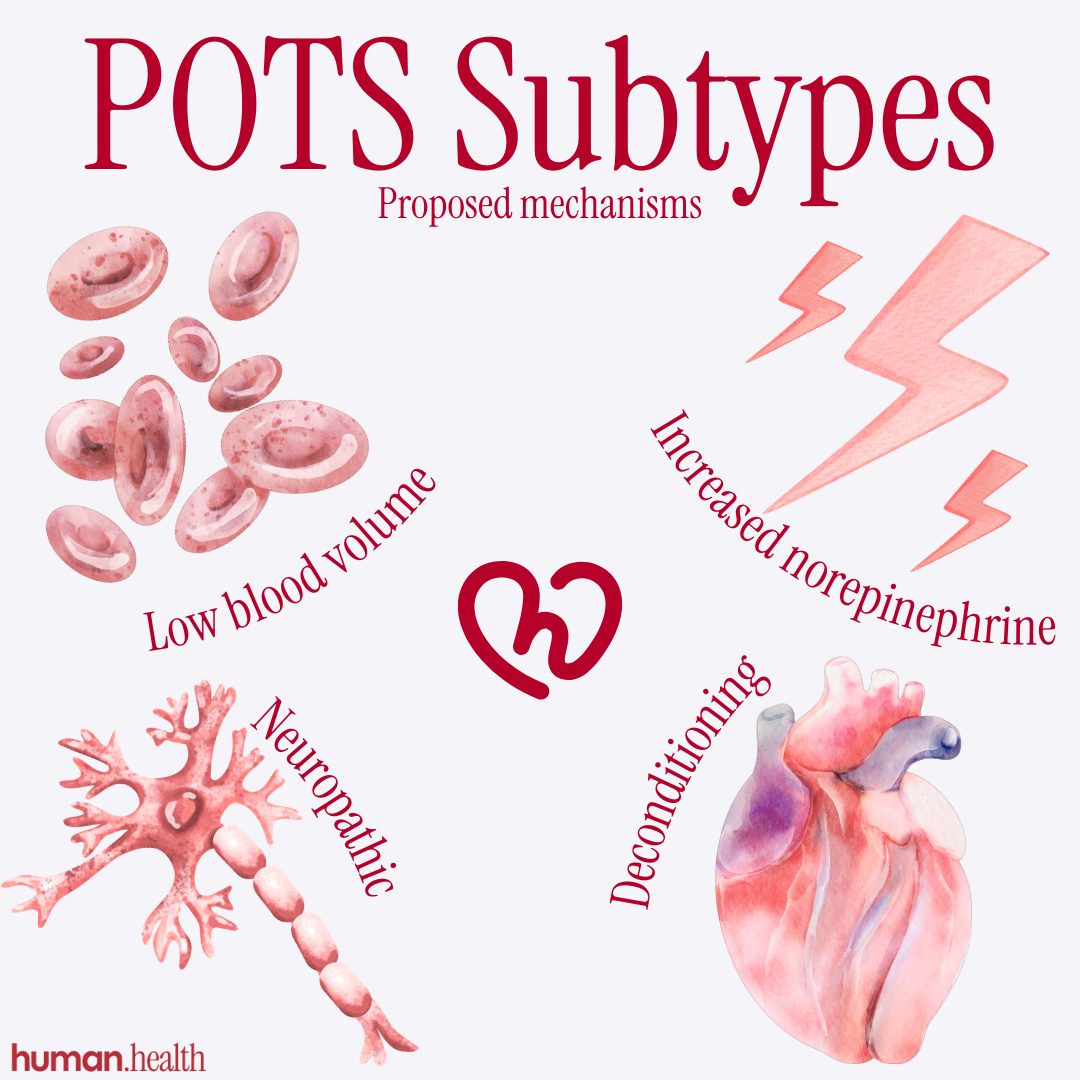
Neuropathic
The autonomic nervous system controls many of the involuntary processes in the body, such as breathing rate, heart rate, and blood pressure.
Some small, hospital-based studies including POTS patients indicate that some people with POTS may have a reduced number of autonomic nerves, or decreased autonomic nerve activity, in their legs and feet.
These nerves contribute to the control of blood pressure by constricting blood vessels in the lower body to push blood back to the upper body, and if they don’t work properly, the heart may be forced to overcompensate by pumping faster and harder, as it does in POTS.
Hypovolemic
Adequate blood volume is required to maintain appropriate oxygen and nutrient delivery to organs and tissues, and if blood volume drops, the organs won’t function properly, which can lead to symptoms like dizziness and fainting, and life-threatening complications if it’s not corrected.
A small study in 2005 found that people with POTS had significantly lower blood volume than people without POTS. Further, mechanisms in the kidney which would usually counter this decrease in blood volume by reabsorbing fluid and electrolytes from the urine were not compensating as they usually would in a person with low blood volume.
High sympathetic activity
The autonomic nervous system is divided into parts, one of these being the sympathetic nervous system, which acts specifically to increase things like heart rate, blood pressure, and breathing rate. Sympathetic nerves release a chemical called norepinephrine to act on organs and tissues like the heart and blood vessels.
A 2019 literature review reported that across multiple small-scale studies, up to 60% of people with POTS may release higher levels of norepinephrine upon standing. Increased norepinephrine could lead to symptoms such as racing heart, tremors, and anxiety, which are commonly experienced by POTS patients.
Impaired heart function
Like any muscle in the body, the heart can lose strength if it’s exposed to long periods of decreased cardiac muscle activity. There are many circumstances that may lead to deconditioning of the heart, including physical inactivity, chronic illness, and even in astronauts who spend lots of time in low-gravity environments.
A deconditioned heart may have structural changes which decrease the amount of blood pumped with each heartbeat. However, it’s not clear if deconditioning is a primary cause of POTS, or secondary to symptoms and processes in POTS patients.
{{inline-cta-1}}
Secondary POTS: When other conditions lead to or overlap with POTS
Researchers suggest that POTS can be primary or secondary. Primary POTS occurs independently of other conditions, and secondary POTS arises as a result of other conditions which affect the nervous and circulatory systems.
Autoimmune conditions
Autoimmune conditions occur when the immune system mistakenly attacks the body’s own cells. A 2018 literature review identified multiple studies with evidence that people with POTS often also have an autoimmune condition, such as celiac disease or systemic lupus erythematosus (SLE).
If you’re living with lupus as well as POTS, using a Lupus tracking app can help you record flares, joint pain, fatigue, and other symptoms so you and your care team can see how they may overlap with your POTS triggers.
Infections
An online survey of 4,835 patients diagnosed with POTS between 2015 and 2017 identified that 41% of patients reported the onset of their symptoms within 3 months of an infection.
In particular, the COVID-19 pandemic has further brought to light a link between viral infections and POTS. In 2023, the Royal Australian College of General Practitioners published a study comparing the autonomic dysfunction between people with POTS and people with persistent complications of COVID-19 (long COVID).
The researchers found that 80% of patients with long COVID had symptoms of POTS indistinguishable from those diagnosed with POTS independently. Although the study was small, it highlights the further need for research to explore the relationship between viral infections and conditions of autonomic dysfunction, including POTS.
Diabetes
People with diabetes may experience complications of the disease that lead to damage of the nerves. Since neuropathic changes are theorized to contribute to the development of POTS, there may be increased risk for developing POTS in patients with diabetes.
You can learn more about the connection between POTS and blood sugar to better understand how glucose levels may influence POTS symptoms.
Hypermobility
Although research is still emerging, some studies have identified that a considerable number of patients with hypermobility syndromes, such as hypermobile Ehlers-Danlos syndrome (hEDS), and other hypermobility spectrum disorders (HSD) may experience symptoms of orthostatic intolerance similar to POTS symptoms. These studies provide limited evidence, and further research is required to confirm the association.
If you’ve experienced both hypermobility and POTS-like symptoms, our Hypermobile Ehlers-Danlos (hEDS) Quiz offers a simple way to reflect on your experiences and explore how these conditions may be connected - helping you prepare for a more informed discussion with your healthcare provider.
Common symptoms across all POTS subtypes
Despite the variation between theories for the causes behind the development of POTS, people with POTS often experience symptoms that are characteristic of the condition, regardless of etiology.
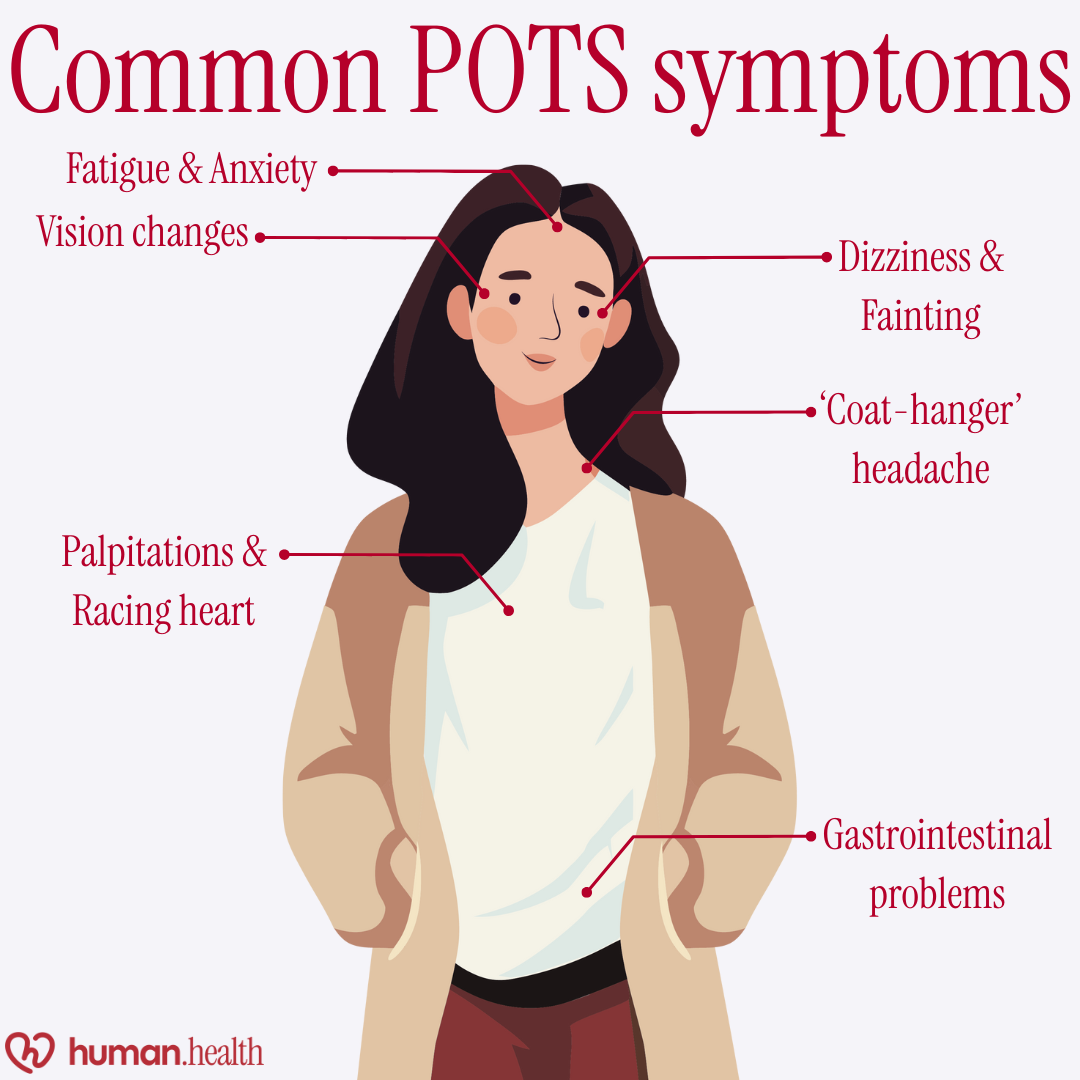
Orthostatic intolerance
The hallmark of POTS, orthostatic intolerance describes the inability of the nervous and cardiovascular symptoms to coordinate the appropriate circulation of blood from the upper to lower body, particularly after moving from a seated or lying position to upright.
The resulting lack of blood flow to vital organs such as the brain and heart can lead to symptoms such as:
- Dizziness or lightheadedness
- Palpitations, or feelings of a racing heart
- Fading or blurry vision
- Feeling as if you are about to faint
- Fainting
- Difficulty concentrating
- Headache, often in a ‘coat-hanger’ pattern across the back of the shoulders and neck
Symptoms of orthostatic intolerance may get worse after lying down or standing still for a long time, in the heat, with dehydration, in the morning, during the menstrual period, and in periods of illness or stress, these situations can often trigger a POTS flare-up.
Fatigue
Experienced as a symptom of many chronic illnesses, fatigue is often reported by patients with POTS. Sleep disturbances could also contribute to worsening fatigue, and some patients report that it is not relieved by rest and can last for days or weeks.
Anxiety
People with POTS may experience anxiety, and sometimes this anxiety is specific to their POTS symptoms. Feelings of anxiety in POTS may be related to increased awareness of and attention to internal sensations and symptoms, as well as fear or anticipation of symptoms.
Read more about the relationship between POTS and anxiety here.
Gastrointestinal problems
It’s unclear why many patients with POTS present with gastrointestinal issues, but common symptoms include nausea, vomiting, constipation, diarrhea, bloating, abdominal pain, and heartburn.
Managing POTS
As we’ve explored, the potential causes and triggers of POTS are complex, and getting symptoms under control can be tricky as a result.
Electrolytes and fluid balance
IIncreasing blood volume by staying hydrated and maintaining adequate electrolyte levels could help regulate blood pressure, to keep orthostatic intolerance symptoms under control.
{{pro-tip-1}}
Sleep
Adopting a regular bedtime routine with good sleep hygiene could also contribute to improving symptoms of fatigue and tiredness.
Read our post about tips and resources for sleep issues for more information about sleep hygiene.
Exercise
Experts claim that people with POTS should avoid sitting or lying down for long periods of time throughout the day to prevent further deconditioning of the cardiovascular system.
Although some patients may find it difficult at the start, beginning to incorporate aerobic exercises that increase the heart rate is recommended, in 30–40 minute sessions across 3 or 4 days per week.
Here’s a notable quote from the 2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of POTS:
“Patients should engage in a regular, structured, graduated, and supervised exercise program featuring aerobic reconditioning with some resistance training for the thighs. Initially, exercise should be restricted to non-upright exercises, including the use of rowing machines, recumbent cycles, and swimming to minimize orthostatic stress on the heart.”
Starting with adding small but impactful habits to your routine, like calf raises, leg crossing, and shifting weight between feet while standing, could help encourage the venous system to pump blood back to the rest of the body.
Individualized exercise plans are important to ensure that exercises are tailored to your health and abilities. Consult with your doctor about the best ways to approach exercise for you.
Compression garments
In addition to other management strategies, wearing compression stockings or abdominal binders could help to reduce blood pooling in the extremities - one of several remedies for POTS that can make daily life more manageable.
When to seek medical attention
You know your body best, and it’s important to listen to your intuition. Seek advice from a medical professional if:
- You are having chest pain or shortness of breath
- Your symptoms aren’t resolving within their usual timeframe
- You are fainting or losing consciousness more than usual, or you hit your head
- You can’t complete activities of daily living, such as eating, going to the bathroom, and moving around independently
{{pro-tip-2}}
Your healthcare provider can give you advice about what symptoms constitute an emergency.
The Human Health app: Manage POTS with ease
The Human Health app is an app designed for patients with chronic and complex diseases like POTS, to make managing your health easier than ever.
Here are a couple of features within the app that can help you:
- Log your symptoms as they happen, and see how they’re impacting you over time
- Plan keeps your treatment record all in one place, with customizable notifications so you never miss a treatment again
- Downloadable reports you can share with your clinician, so you can clearly and confidently communicate how your health is affecting you
- Schedule one-off or recurring appointments, reminders when appointments are coming up, and get reminders when they’re coming up
- Attach notes to symptoms, appointments, treatments, and more, so you can keep track of what’s important to you
The Human Health app was built for people affected by chronic diseases to revolutionize how you understand your health, and to help you learn what works best for you.
FAQs:
1. Can someone have more than one type of POTS?
Yes, the subtypes of POTS can often overlap, and people with POTS may be affected by more than one subtype that could contribute to multifactorial triggers for the condition.
2. Which POTS subtype is most common?
There are conflicts in the scientific literature about which subtype is the most common, and further research is required to determine this.
3. What mimics POTS symptoms?
There are many different conditions that can present similarly to POTS. Some of these include dehydration, medication side effects and interactions, panic and anxiety disorders, hypermobile Ehlers-Danlos syndrome, mast cell activation syndrome, and isolated episodes of increased heart rate, orthostatic hypotension, orthostatic intolerance, and fainting.
For individuals experiencing overlapping symptoms, understanding the link between mast cell activation syndrome and POTS can provide valuable insights into how these conditions may coexist and influence each other.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- National Institute of Neurological Disorders and Stroke. (n.d.). Postural tachycardia syndrome (POTS). National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/postural-tachycardia-syndrome-pots
- Sheldon RS, Grubb BP 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63. doi: 10.1016/j.hrthm.2015.03.029. Epub 2015 May 14. PMID: 25980576; PMCID: PMC5267948.
- Waxenbaum JA, Reddy V, Varacallo MA. Anatomy, Autonomic Nervous System. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539845/
- Peltier, A.C., Garland, E., Raj, S.R. et al. Distal sudomotor findings in postural tachycardia syndrome. Clin Auton Res 20, 93–99 (2010). https://doi.org/10.1007/s10286-009-0045-y
- Singer W, Spies JM, McArthur J, Low J, Griffin JW, Nickander KK, Gordon V, Low PA. Prospective evaluation of somatic and autonomic small fibers in selected autonomic neuropathies. Neurology. 2004 Feb 24;62(4):612-8. doi: 10.1212/01.wnl.0000110313.39239.82. PMID: 14981179.
- Taghavi S, Nassar AK, Askari R. Hypovolemia and Hypovolemic Shock. [Updated 2025 Jun 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513297/
- Raj SR, Biaggioni I, Yamhure PC, Black BK, Paranjape SY, Byrne DW, Robertson D. Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation. 2005 Apr 5;111(13):1574-82. doi: 10.1161/01.CIR.0000160356.97313.5D. Epub 2005 Mar 21. PMID: 15781744.https://www.ahajournals.org/doi/10.1161/01.CIR.0000160356.97313.5D
- UpToDate. (2025). Postural tachycardia syndrome. https://www.uptodate.com/contents/postural-tachycardia-syndrome
- Coupé M, Fortrat JO, Larina I, Gauquelin-Koch G, Gharib C, Custaud MA. Cardiovascular deconditioning: From autonomic nervous system to microvascular dysfunctions. Respir Physiol Neurobiol. 2009 Oct;169 Suppl 1:S10-2. doi: 10.1016/j.resp.2009.04.009. Epub 2009 Apr 18. PMID: 19379845.
- Parsaik A, Allison TG, Singer W, Sletten DM, Joyner MJ, Benarroch EE, Low PA, Sandroni P. Deconditioning in patients with orthostatic intolerance. Neurology. 2012 Oct 2;79(14):1435-9. doi: 10.1212/WNL.0b013e31826d5f95. Epub 2012 Sep 19. PMID: 22993288; PMCID: PMC3525293.
- National Heart, Lung, and Blood Institute. (2021, September 23). Decoding the mysteries of postural orthostatic tachycardia syndrome. National Institutes of Health. https://www.nhlbi.nih.gov/news/2021/decoding-mysteries-postural-orthostatic-tachycardia-syndrome
- Vernino S, Stiles LE. Autoimmunity in postural orthostatic tachycardia syndrome: Current understanding. Auton Neurosci. 2018 Dec;215:78-82. doi: 10.1016/j.autneu.2018.04.005. Epub 2018 Apr 26. PMID: 29909990.
- Shaw BH, Stiles LE, Bourne K, Green EA, Shibao CA, Okamoto LE, Garland EM, Gamboa A, Diedrich A, Raj V, Sheldon RS, Biaggioni I, Robertson D, Raj SR. The face of postural tachycardia syndrome - insights from a large cross-sectional online community-based survey. J Intern Med. 2019 Oct;286(4):438-448. doi: 10.1111/joim.12895. Epub 2019 Apr 16. PMID: 30861229; PMCID: PMC6790699.
- Seeley MC, Gallagher C, Ong E, Langdon A, Chieng J, Bailey D, Page A, Lim HS, Lau DH. High Incidence of Autonomic Dysfunction and Postural Orthostatic Tachycardia Syndrome in Patients with Long COVID: Implications for Management and Health Care Planning. Am J Med. 2025 Feb;138(2):354-361.e1. doi: 10.1016/j.amjmed.2023.06.010. Epub 2023 Jun 29. PMID: 37391116; PMCID: PMC10307671.
- UpToDate. (2025). Epidemiology and classification of diabetic neuropathy. https://www.uptodate.com/contents/epidemiology-and-classification-of-diabetic-neuropathy
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

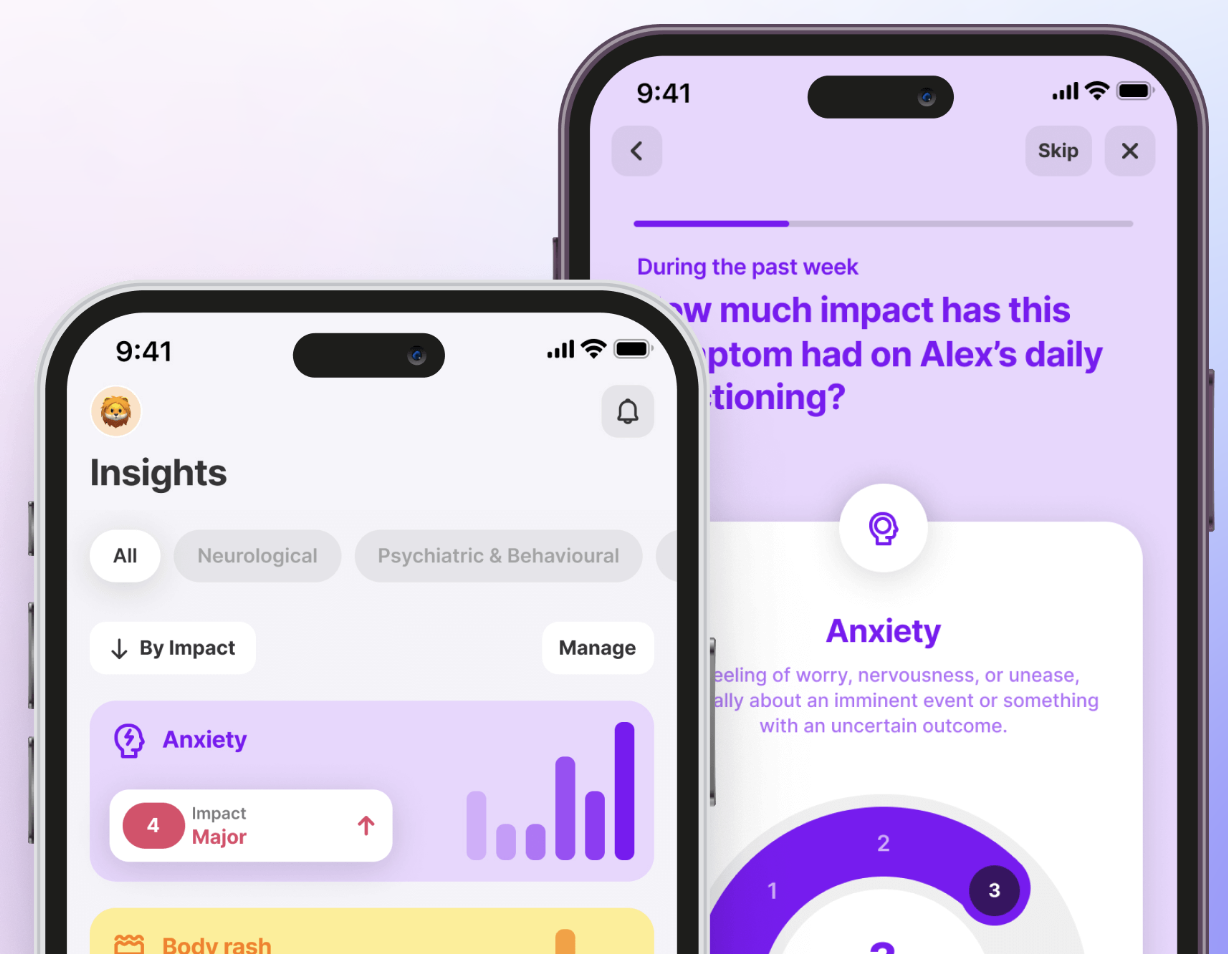
Manage POTS Inside The Human Health App
Inside the Human Health app, you can track dizziness, fatigue, and rapid heart rate all in one place - helping you see patterns, manage flares, and take control of your health with data-driven insights.







Pro tip
Track your fluid and electrolyte intake using an app like Human Health, so you can stay on top of your daily hydration targets
Pro tip
Keeping a log of when and how your symptoms affect you in the Human Health app could make conversations with your healthcare team quicker and clearer

.jpg)




.png)

