Dysautonomia vs POTS: Shared Symptoms & Differences
October 1, 2025
- Dysautonomia is a broad term describing dysfunction of the autonomic nervous system, while POTS (Postural Orthostatic Tachycardia Syndrome) is one specific type of dysautonomia.
- Both conditions may share symptoms like dizziness, fatigue, and heart rate changes, but they are not the same condition.
- POTS is primarily identified by a rapid heart rate increase upon standing, whereas other forms of dysautonomia can affect blood pressure, digestion, or temperature regulation.
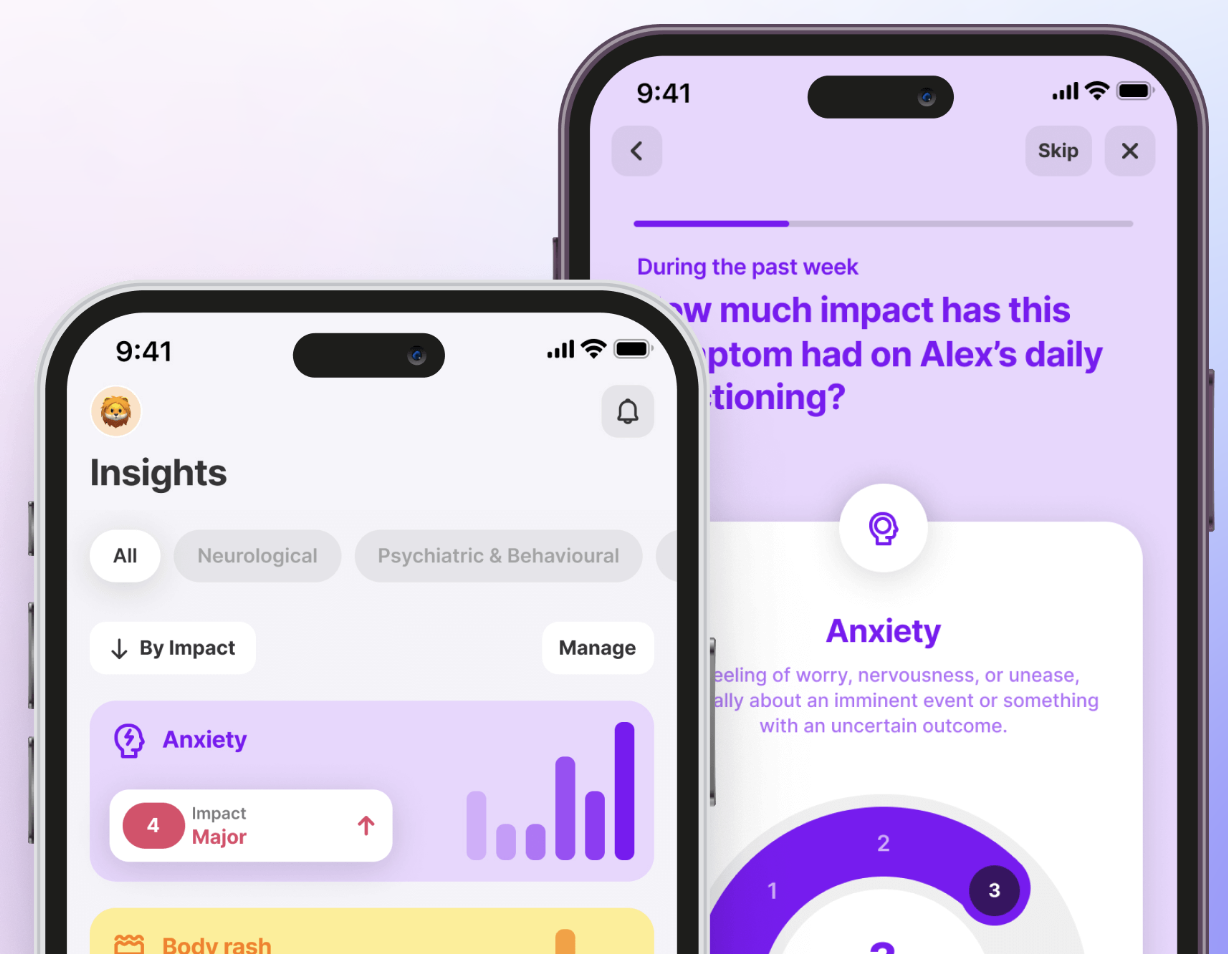
- Using the Human Health App to track daily symptoms, treatment responses, and triggers can help you and your healthcare provider spot meaningful patterns and guide care discussions.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is for educational purposes only and is not a substitute for professional medical advice. Please consult a qualified healthcare provider about your specific situation.
Many people wonder whether they’re dealing with the same condition or two separate health issues when it comes to dysautonomia vs POTS. The answer is that dysautonomia is an umbrella term for autonomic nervous system dysfunction, while POTS (Postural Orthostatic Tachycardia Syndrome) is one specific type defined by a rapid heart rate increase when standing.
In this article, we’ll walk through their shared symptoms, the differences that matter most, how doctors diagnose them, and what current treatments look like. You’ll also learn how tracking with the Human Health app can help you and your provider connect the dots and make more informed care decisions.
What is the link between POTS and dysautonomia?
Dysautonomia refers to any disorder involving altered function of the autonomic nervous system. The autonomic nervous system (ANS) controls functions you don’t usually think about, like heart rate, blood pressure, digestion, and temperature regulation.
POTS (Postural Orthostatic Tachycardia Syndrome) is a specific form of dysautonomia. It is characterized by an excessive increase in heart rate (tachycardia) when moving from lying down to standing up. In other words, all POTS cases fall under dysautonomia, but not all dysautonomia is POTS.
This connection matters because understanding whether symptoms are caused by POTS or another form of dysautonomia can guide the right diagnosis and management approach.
Possible shared symptoms of POTS and dysautonomia
Both conditions can affect the body in similar ways, making them easy to confuse. Here are some symptoms that may overlap:
Dizziness and lightheadedness
Many people with POTS or related dysautonomia experience dizziness (especially upon standing), and in some cases, this can lead to presyncope (near-fainting) or syncope (fainting). Tracking when dizziness occurs in the Human Health App can help identify triggers, such as dehydration, hot environments, or long periods of standing.
Fatigue
Both conditions may cause chronic, significant fatigue, a kind of tiredness that often persists and is not fully relieved by rest. This tiredness can interfere with daily activities and quality of life. Logging energy levels in the app can help you and your healthcare provider understand patterns over time.
Brain fog
Difficulty concentrating, memory lapses, or slowed thinking, often called “brain fog”, are recognized symptoms in POTS and other dysautonomias. These episodes may be linked to blood flow changes in the brain. Recording when brain fog happens can provide valuable data for care discussions.
Rapid heart rate
A rapid heartbeat when standing is the hallmark of POTS, though other forms of dysautonomia can also cause elevated heart rate in certain situations.
While these overlapping symptoms can make it difficult to tell the conditions apart, tracking them consistently gives you and your healthcare provider a clearer view. Recognizing patterns over time is often the first step toward an accurate diagnosis and better management.
What are the differences between POTS and dysautonomia?
While POTS is one form of dysautonomia, not all dysautonomia presents the same way. Here are some key differences:
POTS: Heart rate focused
POTS is defined by a sustained heart-rate increase of ≥30 beats per minute within the first 10 minutes of standing from a lying position, and typically without a significant drop in blood pressure.
Other dysautonomias: Broader autonomic dysfunction
Other forms of dysautonomia affect more than just heart rate. For example, neurally mediated syncope can cause sudden drops in blood pressure and fainting, while multiple system atrophy may disrupt blood pressure, digestion, bladder control, and temperature regulation. These conditions are often more complex and involve several parts of the autonomic nervous system.
Symptom triggers
People with POTS often notice symptoms worsening with prolonged standing, heat exposure, or after large meals. In contrast, other types of dysautonomia often have different triggers — for example, digestive activity or certain environmental temperature changes may worsen symptoms in disorders involving autonomic failure. Recognizing which triggers apply can help healthcare providers narrow down the type of condition.
{{inline-cta-1}}
Age and onset patterns
POTS most commonly develops in premenopausal women, typically beginning in adolescence or early adulthood (and sometimes up to 50 years). Other dysautonomias may develop later in life, particularly in people with chronic illnesses or neurodegenerative disorders such as diabetes or Parkinson’s disease.
You can learn more about the connection between POTS and blood sugar to better understand how metabolic factors may influence symptoms.
These differences highlight the importance of careful evaluation. While symptoms can look similar, identifying what sets POTS apart from other dysautonomias helps guide accurate diagnosis and tailored management strategies.
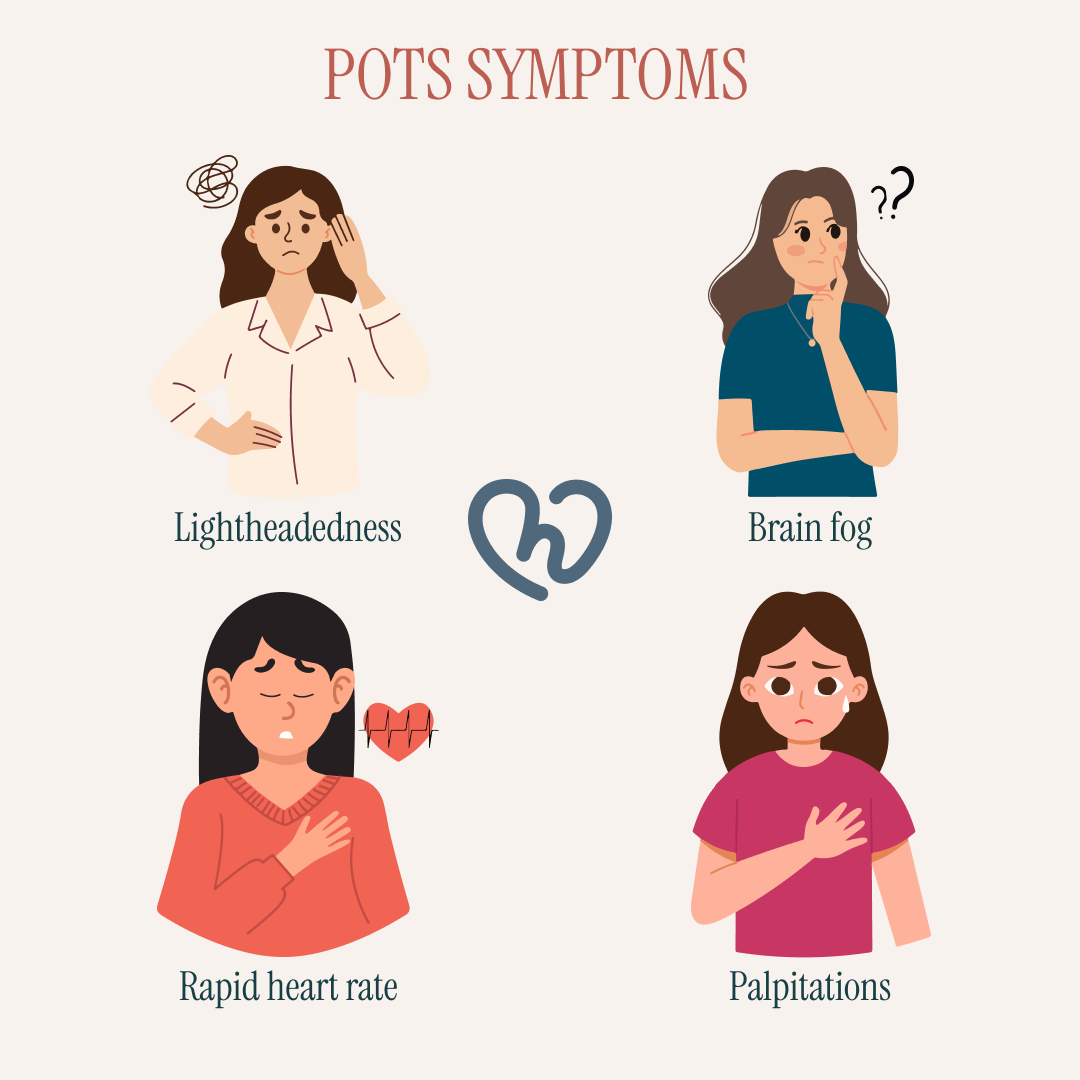
Potential causes of POTS and dysautonomia
Researchers are still studying what drives these conditions, but several contributing factors have been identified.
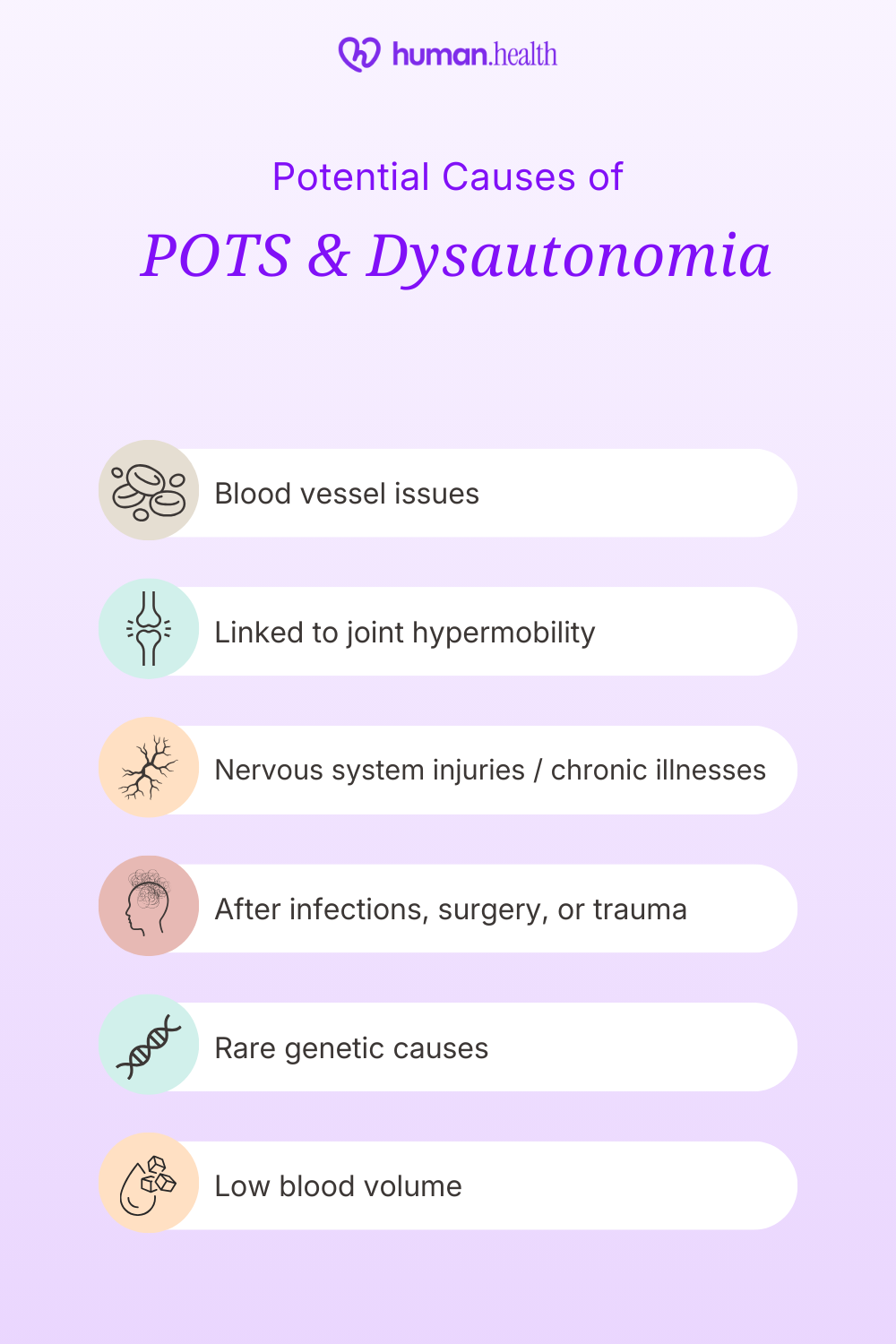
POTS
- Often linked to abnormal blood vessel control, causing impaired vasoconstriction and resulting in blood pooling in the lower body when standing.
- May develop after viral infections, surgery, or trauma.
- Associated with low blood volume, with studies showing up to 70% with decreased plasma, red-cell, or total blood volumes.
- Sometimes overlaps with other conditions such as Ehlers-Danlos syndrome or joint hypermobility. Researchers continue to explore whether POTS is genetic or influenced by inherited factors.
Dysautonomia
- Can occur as a secondary condition linked to diseases such as diabetes or Parkinson’s disease.
- Sometimes develops following injury to the nervous system, such as severe traumatic brain injury.
- Certain rare forms of dysautonomia result from genetic factors, such as autosomal recessive mutations in Familial Dysautonomia.
- Sometimes develops as a result of long-term illnesses that affect the nervous system.
Understanding the potential causes of POTS and dysautonomia highlights how complex these conditions can be. Because triggers and underlying factors vary widely, tracking symptoms and health history can help your healthcare provider piece together the bigger picture and guide more personalized care.
If you’ve noticed joint hypermobility or flexible joints alongside POTS-like symptoms, the Hypermobile Ehlers-Danlos (hEDS) Quiz can help you reflect on your experiences and explore whether hypermobility might be connected to autonomic symptoms — supporting a more informed discussion with your healthcare provider.
How are POTS and dysautonomia diagnosed today? What the studies say
Diagnosing these conditions can be challenging because symptoms overlap with many other health issues. Research shows that delays and misdiagnoses are common, which can make tracking symptoms over time especially valuable.
POTS
A diagnosis is usually considered when symptoms match a specific heart rate pattern.
- Tilt table test (or head-up tilt): The diagnostic criterion requires a heart rate increase of ≥ 30 bpm within the first 10 minutes of standing or tilt in the absence of orthostatic hypotension
- Heart rate monitoring: Wearable devices are increasingly used to monitor heart rate and heart rate variability at home, and early studies suggest they may aid in detecting abnormal upright tachycardia, though they cannot replace formal diagnostic testing
- Symptom history: Detailed clinical history, including the timing of symptom onset and mechanism, is essential in POTS diagnosis to identify consistent triggers.
Dr. Dara K. Lee Lewis, MD, Editorial Advisory Board Member at Harvard Health Publishing, emphasizes the importance of combining practical strategies with real-life adjustments:
“By consistently paying attention to sodium and fluid intake, compression, and exercise... many people who have POTS can successfully attend school and hold down jobs. However, symptoms may flare without warning. Arranging formal accommodations, such as frequent snack breaks and flexible hours, can help people thrive in an academic or work setting.”
Dysautonomia
Dysautonomia covers multiple conditions, so diagnosis varies depending on the subtype.
- Autonomic function testing: Includes measures of cardiovagal, sudomotor, and adrenergic function — for example, tests for sweating (sudomotor), heart rate variability (cardiovagal), and blood pressure responses to provocation.
- Neurological exams: Studies show that confirming autonomic disorders often requires a comprehensive examination, including neurological evaluation, of relevant manifestations.
- Underlying conditions: Identifying underlying conditions, such as diabetes, amyloidosis, or distinguishing Parkinson’s disease from similar disorders, helps clarify the diagnosis of autonomic disorders.
Tracking daily episodes of dizziness, fatigue, or rapid heart rate in the Human Health App can provide a timeline for your healthcare provider, reducing the risk of overlooked patterns.

Management advice for POTS and dysautonomia
While there’s no single cure, many people find ways to reduce the impact of symptoms with consistent management strategies.
#1: Track symptoms and patterns
Keeping a detailed symptom log is one of the most practical steps you can take. With the Human Health App, you can track dizziness, fatigue, and heart rate changes, then export PDF summaries for your healthcare provider. Over time, this makes it easier to spot patterns and triggers that might otherwise be missed.
#2: Focus on hydration and salt intake
Increasing fluid and salt intake, in particular, adopting a high‐sodium diet, has been shown to increase plasma volume and reduce upright tachycardia in POTS patients. These changes should only be made under medical supervision.
#3: Gradual exercise and movement
Structured, progressive exercise programs (e.g., recumbent or semi-upright training) have been shown to improve orthostatic tolerance, functional capacity, and quality of life in POTS patients. Low-impact options like recumbent cycling or swimming reduce strain while helping the body adapt over time.
#4: Lifestyle adjustments
Small changes can make a big difference. Compression garments have been shown to reduce orthostatic tachycardia and improve symptoms in POTS patients. Pacing daily tasks also helps conserve energy. Recording these strategies in the app gives you and your provider clearer insight into what’s working.
Management involves trial and error. By combining medical advice with consistent tracking, you can identify strategies that ease your symptoms and bring more stability to daily life.
How is dysautonomia treated today?
Treatment for dysautonomia varies because it includes several different conditions, but studies suggest that combining medication with lifestyle strategies may improve quality of life.
- A recent review reported that treatment of dysautonomia is largely symptomatic (aimed at managing issues such as blood pressure instability) rather than curing the condition.
- Clinical trials show that midodrine can significantly increase standing blood pressure in some forms of autonomic dysfunction, though patient responses and side effects vary.
- Research emphasizes that treating underlying conditions, such as diabetes, is crucial to reducing symptom burden in dysautonomia.
- Non-drug approaches, such as structured exercise and the use of compression garments, are supported in observational studies for helping reduce symptom burden in POTS and related autonomic disorders.
With the Human Health App, you can log medications, set reminders, and export treatment histories to your healthcare provider, making it easier to track what’s helping and what isn’t.

Available POTS treatments today
Treatment for POTS focuses on managing symptoms and improving daily function. Research shows that outcomes can vary, but certain approaches are consistently supported.
- A recent review of exercise-based interventions in POTS reported that many patients saw improvements in orthostatic symptoms and quality of life from structured training programs.
- Clinical trials indicate that medications like beta-blockers and ivabradine can reduce excessive heart rate in POTS, though response varies among patients.
- Increasing fluid and salt intake is considered a cornerstone strategy in POTS treatment; studies show it can help expand blood volume and reduce symptoms like lightheadedness.
- Non-drug strategies, such as compression garments, are supported by smaller studies in POTS; they have been shown to reduce orthostatic tachycardia and improve symptoms.
For additional strategies that may help relieve symptoms, explore our comprehensive post on natural remedies for POTS.
The Human Health App can support your management plan by helping you track treatment routines, log changes in symptoms, and share clear reports with your healthcare provider.
Manage POTS and dysautonomia with the Human Health app
Dysautonomia and POTS share common ground, but there are some distinctions between them. Recognizing their differences is the key to accurate diagnosis, more effective management, and ultimately, a greater sense of control in daily life.
Tracking your own experiences is a powerful part of that process.
With the Human Health app, you can log symptoms like dizziness, fatigue, or heart rate changes, track them alongside treatments or lifestyle notes, and export clear reports to share with your provider.
Small, consistent tracking can turn scattered symptoms into meaningful insights, giving you and your healthcare team the clarity needed to move forward with confidence.
Start tracking today with the Human Health app.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is for educational purposes only and is not a substitute for professional medical advice. Please consult a qualified healthcare provider about your specific situation.
References
- National Library of Medicine: The Diagnostic Journey of Dysautonomia Patients: Insights from a Patient-Reported Outcome Study
- National Library of Medicine: Postural Orthostatic Tachycardia Syndrome
- ABC Cardiol: Dysautonomia: A Forgotten Condition — Part II
- Frontiers in Neuroscience: Brain fog in neuropathic postural tachycardia syndrome may be associated with autonomic hyperarousal and improves after water drinking
- National Library of Medicine: Dysautonomia: a common comorbidity of systemic disease
- US Cardiology Review: Narrative Review of Postural Orthostatic Tachycardia Syndrome: Associated Conditions and Management Strategies
- National Library of Medicine: Clinical Evidence of Dysautonomia
- National Institute of Neurological Disorders and Stroke: Postural Tachycardia Syndrome (POTS)
- National Library of Medicine: Autonomic Dysfunction
- National Library of Medicine: Postural tachycardia syndrome: multiple symptoms, but easily missed
- Dysautonomia Support Network: Forms of Dysautonomia
- American Brain Foundation: What Is Dysautonomia?
- Nature: Symptom presentation by phenotype of postural orthostatic tachycardia syndrome
- Cleveland Clinic Journal of Medicine: Autoimmunity and postural orthostatic tachycardia syndrome: Implications in diagnosis and management
- National Library of Medicine: Postural Orthostatic Tachycardia Syndrome (POTS): Association with Ehlers-Danlos Syndrome and Orthopaedic Considerations
- MedlinePlus: Autonomic Nervous System Disorders
- National Library of Medicine: Familial Dysautonomia
- Cleveland Clinic: Dysautonomia: What It Is, Symptoms, Types & Treatment
- Journal of Trauma and Acute Care Surgery: Risk Factors Related to Dysautonomia After Severe Traumatic Brain Injury
- MDPI: Wearable Devices for Remote Monitoring of Heart Rate and Heart Rate Variability—What We Know and What Is Coming
- ScienceDirect: Evaluation of postural tachycardia syndrome (POTS)
- National Library of Medicine: Autonomic Function Tests: Some Clinical Applications
- National Library of Medicine: Effect of High Dietary Sodium Intake in Patients With Postural Tachycardia Syndrome
- National Library of Medicine: Exercise and Non-Pharmacological Treatment of POTS
- JACC Journals: Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome
- National Institute for Health and Care Excellence: Orthostatic hypotension due to autonomic dysfunction: midodrine
- MDPI: Current Landscape of Compression Products for Treatment of Postural Orthostatic Tachycardia Syndrome and Neurogenic Orthostatic Hypotension
- Autonomic Neuroscience: Basic and Clinical: The use and effectiveness of exercise for managing postural orthostatic tachycardia syndrome in young adults with joint hypermobility and related conditions: A scoping review
- Frontiers in Neurology: Oral medications for the treatment of postural orthostatic tachycardia syndrome; a systematic review of studies before and during the COVID-19 pandemic
- ScienceDirect: Oral and intravenous hydration in the treatment of orthostatic hypotension and postural tachycardia syndrome
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Track Your Symptoms In Our App
With the Human Health App - you can better understand yourself and your needs, allowing you to talk to your providers with confidence & be heard.








.jpg)




.png)

