Does Physical Therapy Help POTS? What The Studies Say
October 9, 2025

- Physical therapy may support people with postural orthostatic tachycardia syndrome (POTS) by gradually building tolerance to upright activity, improving circulation, and enhancing muscle strength.
- Research suggests that graded, symptom-aware exercise programs may improve quality of life and daily function for some people living with POTS.
- Symptoms can fluctuate, so tracking patterns and working closely with a knowledgeable physical therapist may help identify safe pacing and recovery strategies.
- Using a tool like the Human Health app to log symptoms, activity, and hydration can help you and your healthcare provider understand what is working over time.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is intended to support, not replace, conversations with qualified healthcare professionals.
Living with postural orthostatic tachycardia syndrome (POTS) can make even small movements feel exhausting. Standing up, walking across a room, or completing everyday tasks may cause dizziness, rapid heartbeat, or fatigue. For many people, this unpredictable mix of symptoms can make exercise seem impossible.
The good news is that physical therapy for POTS may help some people rebuild strength and tolerance safely.
Studies suggest that gradual, structured movement can support better circulation, muscle conditioning, and overall stability. In this article, we’ll explore what the research shows, what to expect during sessions, and how to adapt physical therapy to your own needs.
Can physical therapy potentially help with POTS?
Physical therapy may help some people with POTS by gradually building their body’s tolerance to upright movement. This often starts with recumbent (seated or lying) exercises that place less stress on the cardiovascular system before progressing to upright activity.
Research suggests that consistent, graded conditioning programs may support circulation, improve autonomic balance, and enhance daily function over time. The goal is not to “cure” POTS but to help your body adapt more efficiently to position changes and movement. Alongside these approaches, exploring natural remedies for POTS may offer additional ways to manage symptoms holistically.

Working with a physical therapist who understands POTS can make this process safer and more personalized.
How symptoms may fluctuate during physical therapy (and what you might do)
Many people with POTS notice that symptom severity (including heart rate and blood pressure) can vary from day to day. You might have sessions where you feel stable and others where fatigue, dizziness, or rapid heart rate appear sooner than expected. These shifts are normal and can be influenced by factors such as hydration levels, environmental temperature, or time of day, which are known to affect orthostatic responses.
If symptoms increase during therapy, you can try adjusting timing, posture, or session length. Some people also find it helpful to break longer sessions into shorter ones with rest in between, or repeat workouts after illness or missed sessions, as outlined in the structured exercise program for POTS.
Sharing these patterns with your physical therapist or clinician can help them adapt your plan and support steadier progress.

What exercises might be best for POTS patients?
Some people with POTS, and certain types of POTS in particular, may benefit from gradual, structured exercises that reduce strain on the cardiovascular system while supporting strength and stability. These should always be guided by a healthcare provider or physical therapist familiar with the condition.
Recumbent cardio
Gentle recumbent exercises (for example, rowing or recumbent cycling) can help maintain cardiovascular endurance while avoiding the upright posture that triggers POTS symptoms, allowing your body to adjust more gradually. Over time, this may help improve stamina and tolerance for daily activities.
Seated or supported strength work
Strengthening the legs, core, and glute muscles from a seated or supported position may help stabilize blood flow and improve movement confidence. Light resistance bands or gentle bodyweight movements can be used at a pace that respects symptom changes. The goal is to build steady, symptom-aware progress rather than push through fatigue.
Breathing and mobility exercises
Controlled breathing exercises, such as slow abdominal breathing, may help the body relax and support steadier heart rhythms. Pairing these exercises with short rest breaks can also make recovery between sessions more comfortable.
{{pro-tip-1}}
When approached gradually and with professional guidance, these movements may support better overall function and confidence in daily life.
Best practices that may help during physical therapy
Adapting how you approach each session can make physical therapy more manageable and consistent. These best practices may help you reduce POTS flare-ups and build steadier progress over time.
Start low and increase gradually
Small, steady increases in duration or intensity can support long-term improvement while minimizing setbacks. Building patience and pacing early on often makes it easier to sustain activity over time.
Use symptom-guided pacing
Instead of following a fixed schedule, let your symptoms guide when and how you move. If dizziness or fatigue rises, it may help to pause, rest, or modify the position. Keeping a record of these reactions can help your therapist tailor sessions to your comfort level more precisely.
Manage temperature and hydration
Warm environments can sometimes make POTS symptoms worse, so keeping the room cool may help reduce strain. Staying hydrated, or using oral rehydration solutions if recommended, can also support comfort and circulation. Being mindful of temperature and hydration may make your sessions feel easier and more manageable.
Support circulation with gentle aids
Wearing compression garments has been shown to shift pooled fluid from the legs and abdomen back toward the heart, reducing standing heart rate in POTS. Moving slowly from seated to standing positions and using leg pumps or ankle flexes may help your body adjust more easily. Always discuss compression or posture changes with your clinician first.
{{pro-tip-2}}
By listening to your body and working collaboratively with your therapist, you can help create a safe and flexible routine that supports long-term stability.
Track your treatments and symptoms in one place with the Human Health app
Physical therapy can feel unpredictable when symptoms change from day to day. Incorporating health tracking, such as noting your sessions, energy levels, hydration, and recovery can make it easier to notice patterns and understand what helps most over time.
With the Human Health app, you can log exercises, record symptom changes, and share your progress with your healthcare provider. These insights can help you adjust your plan with confidence and clarity.
Use the Human Health app to track your journey, stay informed, and make each session a step toward better stability and self-awareness.
{{inline-cta-1}}
Disclaimer
Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is intended to support, not replace, conversations with qualified healthcare professionals.
References
- National Library of Medicine: Exercise in Postural Orthostatic Tachycardia Syndrome: Focus on Individualized Exercise Approach
- National Library of Medicine: Exercise Interventions in the Management of Postural Orthostatic Tachycardia Syndrome: A Scoping Review
- National Library of Medicine: Diurnal Variability in Orthostatic Tachycardia: Implications for Postural Tachycardia Syndrome
- National Library of Medicine: Exercise and Non-Pharmacological Treatment of POTS
- National Library of Medicine: Deep abdominal breathing reduces heart rate and symptoms during orthostatic challenge in patients with postural orthostatic tachycardia syndrome
- National Library of Medicine: Mechanisms of orthostatic intolerance during heat stress
- National Library of Medicine: The Benefits of Oral Rehydration on Orthostatic Intolerance in Children with Postural Tachycardia Syndrome
- National Library of Medicine: One Size Does Not Fit All: An Exploration of Compression Garment Use in Patients With Postural Orthostatic Tachycardia Syndrome
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

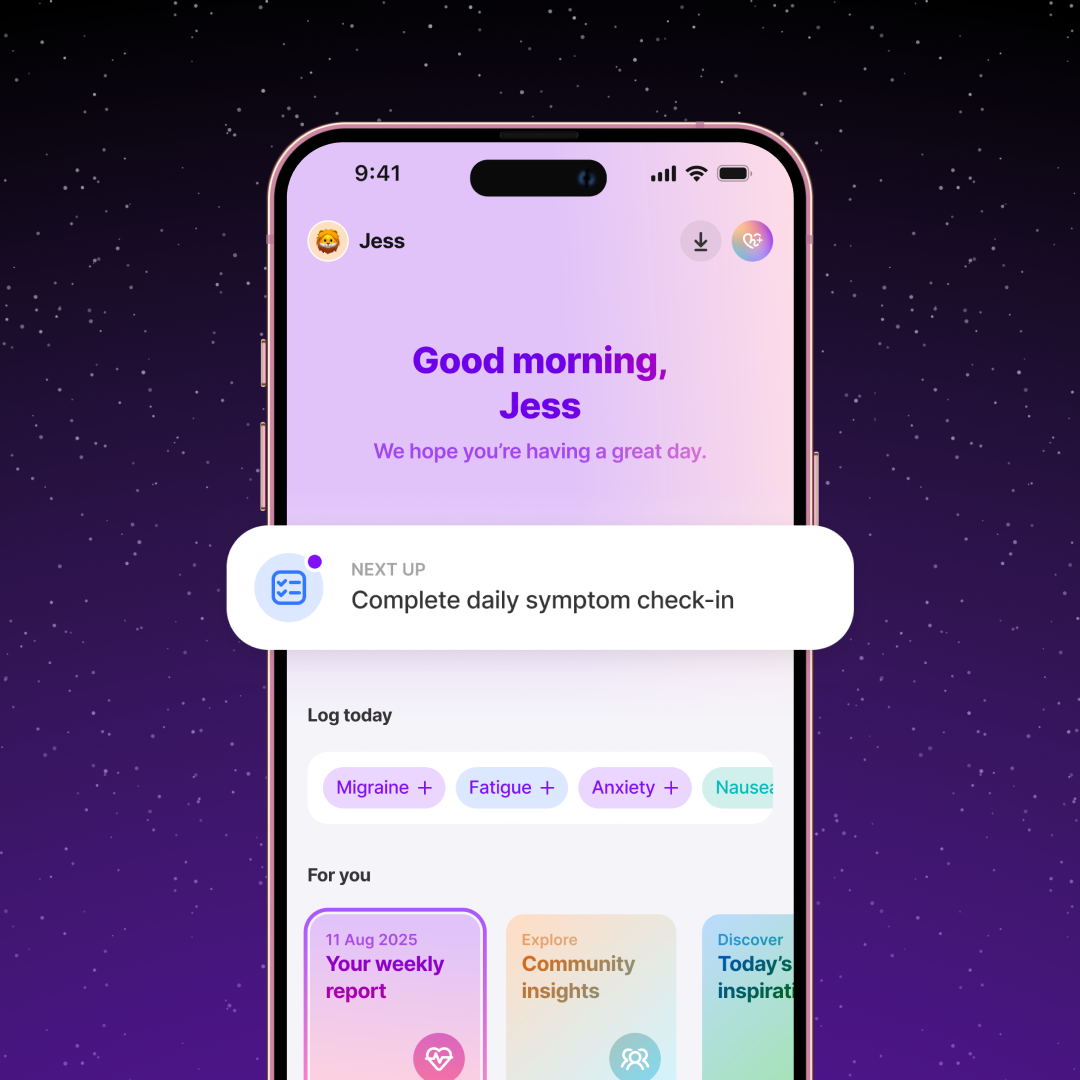
Monitor Your Health Condition Anytime
Track symptoms, log notes, and set daily reminders for all your treatments using the Human Health app.







Pro tip
Cool down slowly after sessions
Taking a few minutes to move gently or practice calm breathing after each session may help your body adjust to position changes and reduce post-session fatigue. Small transitions can make each session feel steadier and more comfortable.
Pro tip
Log how you feel, not just what you do
Noting how your symptoms change before and after each session can reveal useful patterns over time. This helps you and your healthcare team understand which conditions or activities support your best recovery days.

.jpg)




.png)

