POTS Flare-Up: Triggers, Symptoms, & How to Cope
September 2, 2025

- A POTS flare-up is when symptoms temporarily worsen, often triggered by stress, illness, heat, dehydration, or hormonal changes.
- Flare-ups can last anywhere from a few hours to several weeks, depending on the individual.
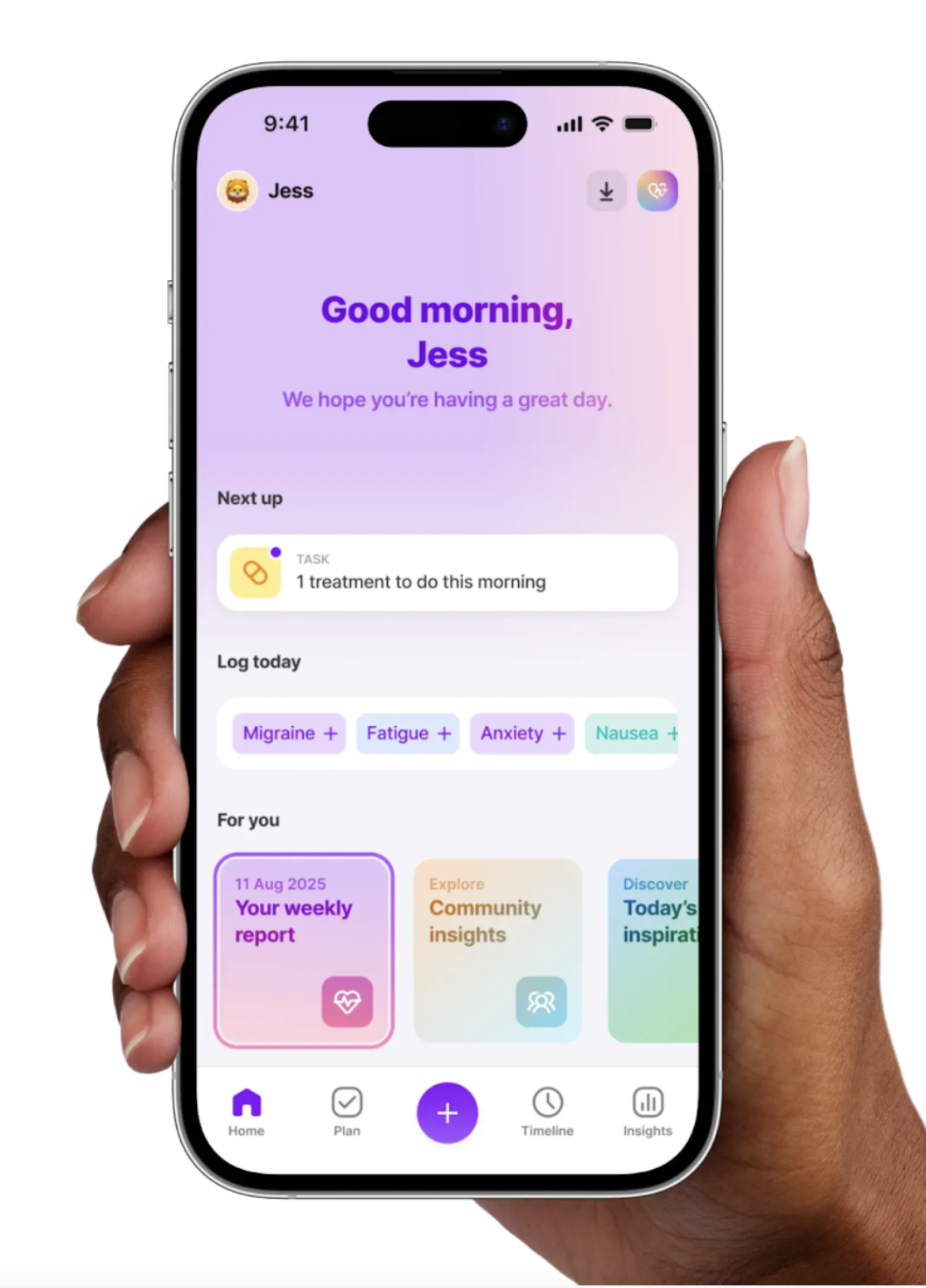
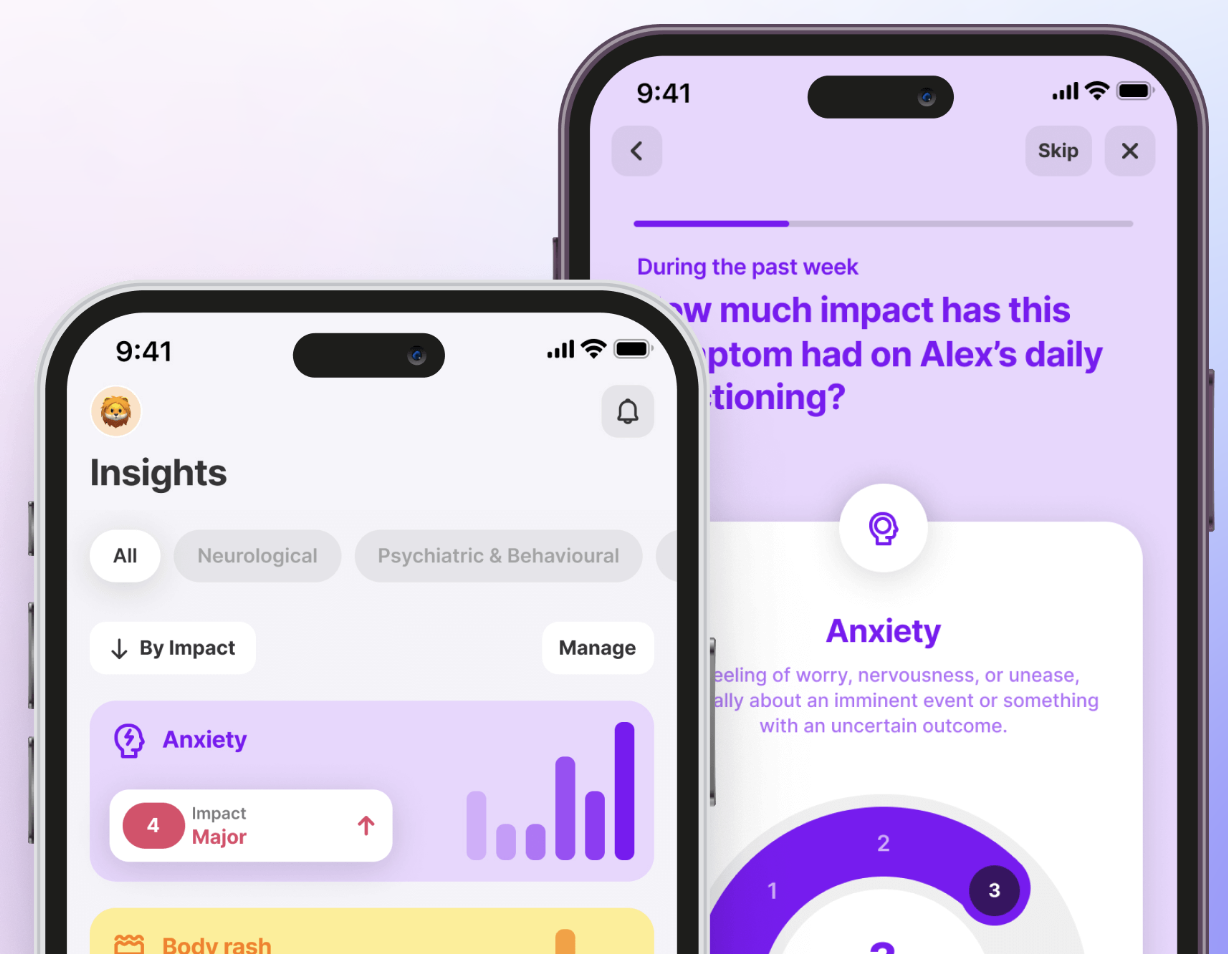
- Using tools like the Human Health app makes it easier to spot patterns, share information with your doctor, and build better coping strategies.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information below is for educational purposes only and is not a substitute for professional medical care. Always consult your doctor or healthcare provider with questions about your health.
Living with POTS can feel overwhelming. Some days you manage your symptoms well, while other days a sudden flare-up makes even simple tasks exhausting. These episodes often bring a surge of dizziness, rapid heartbeat, or fatigue that can disrupt daily life.
Flare-ups may be sparked by things like illness, dehydration, stress, or hormonal changes. In this article, we’ll walk through what happens during a flare, how long it may last, common triggers, and practical ways to track and cope with them so you feel less alone in the process.
What happens during a POTS flare-up?
A flare-up in postural orthostatic tachycardia syndrome (POTS) is when symptoms suddenly worsen beyond your usual baseline. While everyday POTS symptoms might include lightheadedness, rapid heartbeat when standing, or fatigue, a flare is more intense and disruptive.
During a flare, you may experience:
- Dizziness or near-fainting that’s stronger than usual
- Racing heart rate even with minimal activity
- Extreme fatigue or “crash” episodes
- Brain fog and difficulty concentrating
Flare-ups vary widely: for some individuals, they may be brief and mild, while for others they may be more severe and long-lasting.
How long do POTS flare-ups typically last?
The length of a POTS flare-up can differ greatly from person to person. Some people notice their symptoms ease within a few hours, while others experience setbacks that last for days or even weeks. Factors like illness, hormonal changes, and stress levels can all influence recovery time.
Common triggers that can lead to a flare up
Flare-ups often happen when your body is under added strain. While triggers vary, many people with POTS report the following:
Illness or infection
Even a minor infection (e.g., a cold or stomach bug) can trigger worsening of POTS symptoms such as dizziness, fatigue, or tachycardia, and recovery may take longer than in people without POTS.
Heat exposure
Warm environments can make it harder for the body to circulate blood effectively, which may cause less blood to reach the heart and brain. Research shows that heat can lower the body’s ability to stay upright by affecting how blood vessels tighten and relax. Hot weather, saunas, or even long showers may increase dizziness and tiredness for some people with POTS.
Dehydration
When you do not get enough fluids or electrolytes, blood volume can drop, which may make symptoms like lightheadedness and a fast heartbeat worse in POTS. Dehydration may come from sweating, not drinking enough water, or illnesses that cause fluid loss. Staying mindful of hydration levels can reduce the likelihood of sudden worsening.
Hormonal changes
Many women report flares tied to menstrual cycles, pregnancy, or menopause, when changes in estrogen and progesterone affect blood volume and vessel tone. These shifts can make otherwise manageable symptoms much harder to handle during certain times of the month.
Stress and exertion
Periods of high emotional or physical stress (including intense exercise or anxiety) are often cited as triggers for worsening fatigue, dizziness, or palpitations in POTS.
Using the Human Health app, you can log when flares happen and what you were doing beforehand. Over time, this tracking helps reveal personal patterns you can discuss with your doctor.
Symptoms tracking for staying on top of flare-ups
Tracking symptoms turns scattered experiences into clear patterns you can act on. Over time, these insights help you anticipate flare-ups, understand your body, and have more productive conversations with your healthcare provider.
Method #1: Human Health app
The Human Health app was built for complex conditions like POTS. You can log daily symptoms, flare severity, and possible triggers all in one place. Over weeks and months, the app organizes your entries into clear trends, helping you see what makes symptoms better or worse. With one tap, you can export a practitioner-ready PDF summary, transforming vague memories into data-backed insights that support better care decisions.
Method #2: Symptom journal
A notebook or digital diary can be a helpful starting point. Recording when flares begin, what you ate, how much sleep you got, or how stressed you felt can reveal useful connections. However, journals are harder to analyze over time and difficult to share in a structured way with your doctor, where digital tools like the Human Health app offer a big advantage.
Method #3: Wearables and devices
Smartwatches and fitness trackers can add objective data to your records. By logging heart rate spikes, step counts, or sleep quality, you gain another layer of context. When combined with your symptom notes or app entries, this extra data can help you and your provider see how daily activities influence flare intensity.
While any form of tracking is better than none, using a platform designed for complex conditions makes the process easier and more impactful. The Human Health app combines the flexibility of a journal with structured reports and insights you can actually act on, helping you move from feeling overwhelmed by flare-ups to feeling more in control of them.
{{inline-cta-1}}
What to do during a POTS flare-up
When a flare hits, even simple activities can feel overwhelming. Small, supportive adjustments can make the experience more manageable. While every person’s approach is different, many find the following strategies helpful:
Rest and pacing
During a flare, slowing down can make a difference. Lying flat, raising your legs, or breaking activities into smaller steps may ease symptoms related to standing. Resting when needed is not a sign of weakness. It is a way of protecting your body and allowing it to recover.
Cooling and hydration
Staying cool and hydrated can also help you manage flares. Using a fan, a cooling towel, or sipping cold fluids may reduce dizziness or tiredness. Drinks that include electrolytes can help replace fluids, especially if dehydration plays a role.
Supportive positioning
Adjusting your position can sometimes lessen the intensity of symptoms. Elevating your legs on a pillow, wearing compression garments, or using a reclining chair may help blood flow return to the heart. Research suggests that full compression garments can reduce heart rate increases when standing in people with POTS.
“Rest in a reclined position, hydrate with electrolytes, eat small salty meals, and reduce physical and emotional stress. Give your body time to reset.” Dr Cynthia Thiak
Quick Flare Toolkit
- Refillable water bottle or electrolyte drink
- Cooling towel, handheld fan, or ice pack
- Compression socks or leggings
- Reclining chair or pillow for leg elevation
- Notebook or app to log flare details
How to cope with POTS flare-ups
Managing POTS over the long term means building habits that support stability and resilience between flares. These approaches don’t prevent flares entirely but may help reduce their impact.
Building daily routines
Consistent sleep, balanced meals, and gentle activity can create a steadier baseline, making it easier to recover when symptoms spike.
Hydration and salt tracking
Some people choose to monitor their daily fluid and salt intake to see how it relates to their symptoms. Tracking these patterns can help you and your healthcare provider understand whether changes in hydration or salt levels influence how you feel. The Human Health app allows you to log these habits via our Treatment Tracker, track streaks, and share trends with your doctor.
Compression and movement logging
Regular use of compression wear or gentle exercises can be logged to see how they align with symptom changes. Tracking this over time gives a clearer picture of what supports your body best.
When to seek medical attention during a flare-up
It’s important not to dismiss severe or unusual symptoms as “just another flare.” If you experience fainting, chest pain, extreme shortness of breath, or symptoms that feel very different from your usual pattern, seek medical care right away. Only a doctor can rule out other causes and ensure your safety.
What to tell your doctor during a flare
- When the flare started and how long it has lasted
- The main symptoms and how they differ from your baseline
- Any potential triggers you noticed (illness, stress, heat, dehydration)
- Notes or symptom logs from your tracking app or journal
How the Human health app can help you manage POTS flare-ups
Flare-ups often feel unpredictable and frustrating. The Human Health app helps take away some of that uncertainty by showing you what is really happening over time. Logging symptoms, treatments, and routines builds a clear record that you can look back on, rather than guessing.
With practitioner-ready summaries, you arrive at appointments prepared. This makes it easier for your doctor to see the full picture. Tracking habits like hydration, salt intake, or compression wear also gives you clarity on what supports you best, so you can focus energy where it matters most.
Just as your flare toolkit helps you get through the tough moments, the Human Health app gives you a long-term support system. It helps you move from feeling reactive to feeling more in control.
Frequently Asked Questions:
1. Can emotional stress alone cause a POTS flare-up?
Yes. Many people report that emotional stress can trigger or worsen symptoms, though the intensity and duration vary by individual.
2. Should I adjust my exercise routine during a flare?
It’s often helpful to reduce intensity or take a break during a flare, but only a healthcare provider can guide what’s safe for you.
3. Is it normal for flare-up triggers to change over time?
Yes, triggers may shift depending on factors like hormones, illness, or lifestyle. Tracking helps you notice and adapt to these changes.
Sources:
- National Library of Medicine: Cognitive and Psychological Issues in Postural Tachycardia Syndrome
- National Library of Medicine: Menstrual Cycle Affects Renal-Adrenal and Hemodynamic Responses during Prolonged Standing in the Postural Orthostatic Tachycardia Syndrome
- National Library of Medicine: Experiences of living with postural tachycardia syndrome
- National Library of Medicine: Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: a case series of 20 patients
- National Library of Medicine: Postural Orthostatic Tachycardia Syndrome
- Heart and Mind: Psychological stress in postural orthostatic tachycardia syndrome: A pilot pre-COVID survey
- National Library of Medicine: Mechanisms of orthostatic intolerance during heat stress
- National Library of Medicine: Diagnosis and management of postural orthostatic tachycardia syndrome
- ScienceDirect: Oral and intravenous hydration in the treatment of orthostatic hypotension and postural tachycardia syndrome
- JACC Journals: Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome
- National Library of Medicine: Exercise and Non-Pharmacological Treatment of POTS
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Doctors Dismissing You? The Human Health App Doesn't!
Inside the app, you can track all your symptoms, medications, flare ups & more. The app also provides you with insights, so you gain the clarity you need.








.jpg)




.png)

