POTS and PCOS: Links, Symptoms & Differences
December 23, 2025

- Some research suggests a link between POTS and PCOS, mainly because both conditions can involve increased activity in the part of the nervous system that controls stress responses.
- Studies have shown that some people with PCOS experience a faster heart rate when they stand up, which looks similar to POTS.
- A survey of young women with POTS found that around 10 percent also had PCOS, which is similar to the general population. This means PCOS itself is not more common in people with POTS, but symptoms often linked to PCOS are still frequently reported.
- Recognising how hormonal changes and nervous system activity overlap may help you describe symptom patterns more clearly when speaking with your healthcare provider.
Disclaimer: This guide is for informational purposes only. It is not medical advice and should not be used to diagnose, treat, or manage any condition. Always speak with a doctor or qualified healthcare provider about any symptoms or health concerns.
If you’ve noticed symptoms that seem to overlap between POTS and PCOS, it’s understandable to wonder how the two might be connected.
Research shows there may be a connection between POTS and PCOS, mainly through changes in the part of the nervous system that controls heart rate and stress responses.
In this guide, you’ll learn how these conditions overlap, which symptoms they share, and how understanding this relationship can help you prepare for conversations with your healthcare provider.
Is there a link between POTS and PCOS?
Yes, research shows that there could be a meaningful link between POTS and PCOS, mainly through changes in the autonomic nervous system.
Both conditions are associated with increased activity of the sympathetic nervous system, which is responsible for the body’s stress response.
Studies also show that some people with PCOS have a faster heart rate when standing, similar to the pattern seen in POTS episodes.
In a survey of 169 young women with POTS, 10 percent also had PCOS, and many reported symptoms often associated with PCOS, such as acne, irregular periods, and coarse dark hair growth.
How PCOS might affect POTS
PCOS may influence POTS symptoms because it is linked to changes in how the body handles insulin and controls heart rate and stress responses. These changes are connected to increased “fight or flight” activity, which is also linked to the fast heart rate some people experience when standing with POTS.
In one study, people with PCOS had a faster pulse when standing compared to lying down, without a major drop in blood pressure. This response is similar to the pattern seen in POTS and may help explain why some people experience overlapping symptoms.

Shared symptoms between POTS and PCOS
Some people notice overlapping symptoms when living with both POTS and PCOS. These similarities appear in both physical symptoms and in how the nervous system functions. Here are the shared symptoms and features research has found:
Fatigue
Fatigue is very common in POTS and affects more than 90 percent of people in some studies. It was also reported as a frequent premenstrual symptom among those with POTS, which aligns with how hormonal changes can affect people with PCOS.

Acne
People with POTS in survey data reported acne as a common premenstrual symptom. Severe acne is also a recognized sign of higher reproductive hormone levels in PCOS.
Excess hair growth
Coarse dark hair growth was reported by 29.6 percent of people with POTS in one small survey. This is also a key clinical sign used when diagnosing PCOS.
Headaches or migraines
Around 40 percent of people with POTS report headaches, most often migraines. People with POTS have also noted headaches as a frequent premenstrual symptom, which can overlap with patterns of headaches experienced in PCOS.
Menstrual irregularities
About a third of people with POTS in a small survey reported inconsistent menstrual cycles, and many experienced symptom changes around their period. Irregular menstrual cycles are also one of the main ways PCOS is diagnosed.
Anxiety or mood changes
Anxiety is often experienced by people with POTS. Mood changes, such as irritability, were often reported before a period, which also overlaps with symptom presentation in PCOS.
Ovarian cysts
A small study reported that ovarian cysts were experienced by 21 percent of people with POTS. Ovarian cysts are also a common feature of PCOS.
Excessive sweating
Excessive sweating can occur in POTS due to changes in how the nervous system functions. It is also sometimes linked to hormone changes in PCOS.
These overlaps do not mean the conditions always occur together, but recognising them may help you understand patterns in your symptoms and discuss them more confidently with your healthcare provider.
{{pro-tip-1}}
Managing POTS and PCOS together
Living with both POTS and PCOS can feel challenging because symptoms can overlap, change over time, and be hard to explain during medical appointments. Because both conditions affect the body’s stress response, it may help to talk with your healthcare provider about everyday habits that support overall stability.
Prioritise supportive aerobic activity
Gentle aerobic exercise that doesn’t involve standing upright has been studied in POTS and may help support heart rate and blood flow stability. Similar types of exercise have also been explored in PCOS and may support more balanced nervous system activity.
You can use the Human Health app to log exercise sessions and note how your symptoms respond over time.
Support hydration and salt intake with your healthcare provider
Hydration and salt intake are often discussed in the context of POTS to support blood volume. Because needs vary, it is important to check with your healthcare provider before making changes.

Consider compression
Waist-high compression garments may help reduce blood pooling when upright, which can support stability when standing.
{{pro-tip-2}}
Look into sleep health
People with PCOS are more likely to experience sleep problems such as sleep apnea, which can affect how the body responds to stress. If you notice ongoing sleep issues, it may be helpful to raise them with your healthcare provider.
Discuss endocrine and metabolic support
Insulin resistance is common in PCOS and occurs when the body’s cells become less responsive to insulin, a hormone that helps regulate blood sugar. Over time, this can lead to higher insulin and glucose levels in the blood, which may affect energy levels, weight regulation, and hormone balance, as well as the body’s stress response.
Explore hormonal support
Some people with POTS notice that symptoms change around their menstrual cycle. In survey data, some people who used hormonal contraception for cycle-related changes reported improvement. Tracking these patterns in the Human Health app can help you bring clearer information to your appointments.
Understanding these shared patterns can help you prepare for more informed discussions with your healthcare provider and recognise how POTS and PCOS may interact in day-to-day life.
When should you see a doctor?
If you live with POTS, PCOS, or both, it is important to speak with a doctor if your symptoms are becoming harder to manage or begin to affect your daily activities. You should also seek medical advice if you notice new symptoms, changes in your menstrual cycle, or if your heart rate or lightheadedness feels different from what you usually experience.
A doctor can help rule out other causes, review your overall health, and guide you through options that may be appropriate for your individual situation.
{{inline-cta}}
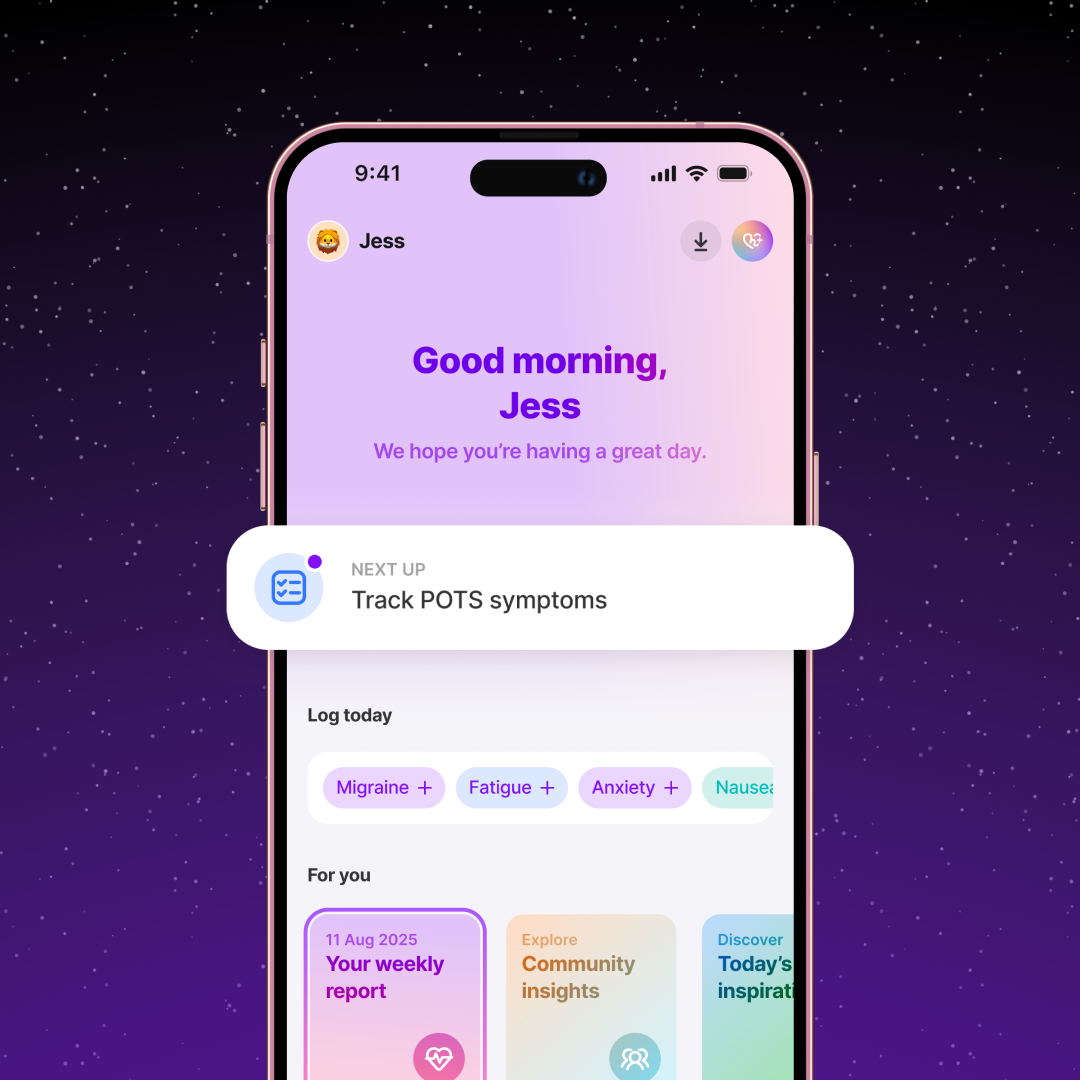
Track hormonal triggers and POTS flares using the Human Health app
Symptoms in both POTS and PCOS may shift with hormones, sleep, stress, and daily routines, and keeping track of these changes can help you understand your own patterns more clearly.
The Human Health app lets you log symptoms, periods, and daily habits in one place so you can bring clearer, more organised information to your healthcare appointments.
If you want a simple way to understand what affects your symptoms and feel more prepared when speaking with your doctor, try the Human Health app. Tracking what you experience day to day can make a real difference in how confidently you navigate both conditions.
References
Raj SR, Fedorowski A, Sheldon RS. Diagnosis and management of postural orthostatic tachycardia syndrome. CMAJ. 2022;194(10):E378–E385. Doi: https://doi.org/10.1503/cmaj.211373
Bourne KM, Connolly SJ, Sheldon RS, Raj SR. The Long-Term Postural Orthostatic Tachycardia Syndrome Outcomes Study. J Am Heart Assoc. 2025;14(15):e034567. doi:
https://doi.org/10.1161/JAHA.124.034567
Yıldırım BA, Ayhan S, Karaca Z, et al. Autonomic dysfunction in women with polycystic ovary syndrome. Clin Endocrinol (Oxf). 2015;83(3):434–441. doi:
https://doi.org/10.1111/cen.12745
Amirana M, Nivedita N, Ramesh S, et al. Characteristics of heart rate variability in women with polycystic ovary syndrome. J Clin Diagn Res. 2018;12(9):CC01–CC05. doi:
https://doi.org/10.7860/JCDR/2018/36312.12023
Xiong Y, Zhang X, Li Y, et al. The role of the autonomic nervous system in polycystic ovary syndrome. Front Endocrinol (Lausanne). 2024;15:1295061. doi:
https://doi.org/10.3389/fendo.2023.1295061
Disclaimer
The Human Health app is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with your healthcare provider.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Track your POTS symptoms with the Human Health app
Log symptoms and interventions to discover the unique patterns that help you drive more safely.







Pro tip
Track symptoms around hormonal shifts:
Many people with POTS report symptom changes before or during their period, and menstrual irregularities are also a key feature of PCOS. Tracking your symptoms and menstrual symptoms side by side can help you notice whether certain phases of your cycle affect how you feel. Bringing this information to your healthcare provider can support clearer, more personalized discussions.
Pro tip
Log upright vs. resting symptoms to spot patterns
Both POTS and PCOS have been linked to differences in how the body responds when standing. Noting how your symptoms change between resting and upright positions can help you understand what triggers flare-ups. Keeping these details organised in one place makes it easier to explain your experience during medical appointments.

.jpg)




.png)

