Can Smoking Cause POTS Syndrome? Effects, Risks, and Advice
January 15, 2026
- Nicotine from cigarettes and e-cigarettes can interfere with the autonomic nervous system, which controls heart rate and blood vessel function. This same system is disrupted in POTS.
- Research suggests that nicotine exposure, including from long-term vaping, can affect how the autonomic nervous system regulates heart rate. These effects have been observed in the general population, not just in people with POTS.
- Current evidence does not show that smoking or vaping causes POTS. No direct causal link has been established.
- Only a doctor can diagnose POTS. Tracking symptoms may help you notice patterns related to nicotine use to discuss with your healthcare provider, but it cannot confirm a diagnosis.
Disclaimer: This guide is for informational purposes only. It is not medical advice and should not be used to diagnose, treat, or manage any condition. Always speak with a doctor or qualified healthcare provider about any symptoms or health concerns.
If you experience symptoms like dizziness or a fast heart rate when standing, smoking may raise concerns.
You may be asking: can smoking cause POTS syndrome? The short answer is no. Smoking is not known to cause POTS.
In this article, you will learn what is known about nicotine, the autonomic nervous system, and why these effects may still be worth discussing with your doctor.
Can smoking cause or trigger POTS?
There is no research confirming smoking or vaping as a cause of POTS. What is known is that POTS involves the autonomic nervous system, which controls heart rate and blood pressure.

Nicotine from cigarettes and e-cigarettes is linked to changes in this same system, including signals that increase heart rate and affect blood vessels.
Because both POTS and nicotine exposure affect autonomic regulation, nicotine use may be relevant to discuss when symptoms are present. This does not mean that smoking leads to POTS.
Only a doctor can determine whether symptoms are related to POTS or another condition.
How might nicotine affect the autonomic nervous system?
Nicotine is linked to changes in how the autonomic nervous system works. This system controls automatic functions like heart rate and blood pressure. Because POTS also involves this system, nicotine exposure may be relevant to discuss with a healthcare provider if you have or suspect you may have the condition.
Increased sympathetic activity
Nicotine exposure is associated with increased sympathetic activity in the autonomic nervous system. This means the body shifts toward a more activated, fight-or-flight state. In some people, that can lead to a faster heart rate, changes in blood pressure, sweating, trembling, or a sense of restlessness.
Changes in heart rate variability
Research has found changes in heart rate variability after nicotine exposure, meaning that the amount of time between heart beats varies more. This could reflect changes to the way the autonomic nervous system controls the heart.
Short-term versus ongoing effects
Scientific evidence describes both short-term and longer-term changes in autonomic balance linked to nicotine exposure. Some studies report autonomic changes even after a period without recent nicotine use.
Vaping-related autonomic changes
Studies of habitual e-cigarette users report a shift toward sympathetic predominance, meaning the body spends more time in a fight-or-flight state, compared with non-users.
Areas where evidence is limited
There is limited research on how nicotine withdrawal, symptoms that return or temporarily feel worse after stopping nicotine, or blood flow to the brain relate to autonomic symptoms.
{{pro-tip-1}}
Can vaping also affect POTS symptoms?
Current evidence does not show that vaping causes POTS or directly affects POTS symptoms.
Studies comparing electronic cigarettes and traditional cigarettes suggest that nicotine is the main factor behind autonomic changes in cigarette smokers.
Some research has found that older e-cigarette devices may have less severe short-term cardiovascular effects than traditional cigarettes, but this does not mean vaping is risk-free.
Research on vaping continues to evolve, especially with newer, high-nicotine products. More studies are needed to understand how vaping may relate to autonomic symptoms and whether these effects differ for people with POTS.
Could smoking make POTS treatment less effective?
There is no direct evidence showing that smoking makes POTS treatments less effective.
Nicotine affects the autonomic nervous system, which many POTS treatments focus on, so this may be important to discuss with your doctor when reviewing medications and symptom control.
Tips for managing POTS if you smoke
If you smoke and are dealing with symptoms that affect your heart rate or balance, it can feel difficult to know which symptoms require medical attention. Research is limited, but staying observant and working closely with your healthcare provider can help guide next steps.
1. Focus on observation, not conclusions
You may notice that symptoms feel different at certain times of day or around nicotine use. This does not mean smoking is the cause, but noting patterns can provide useful context for medical discussions.
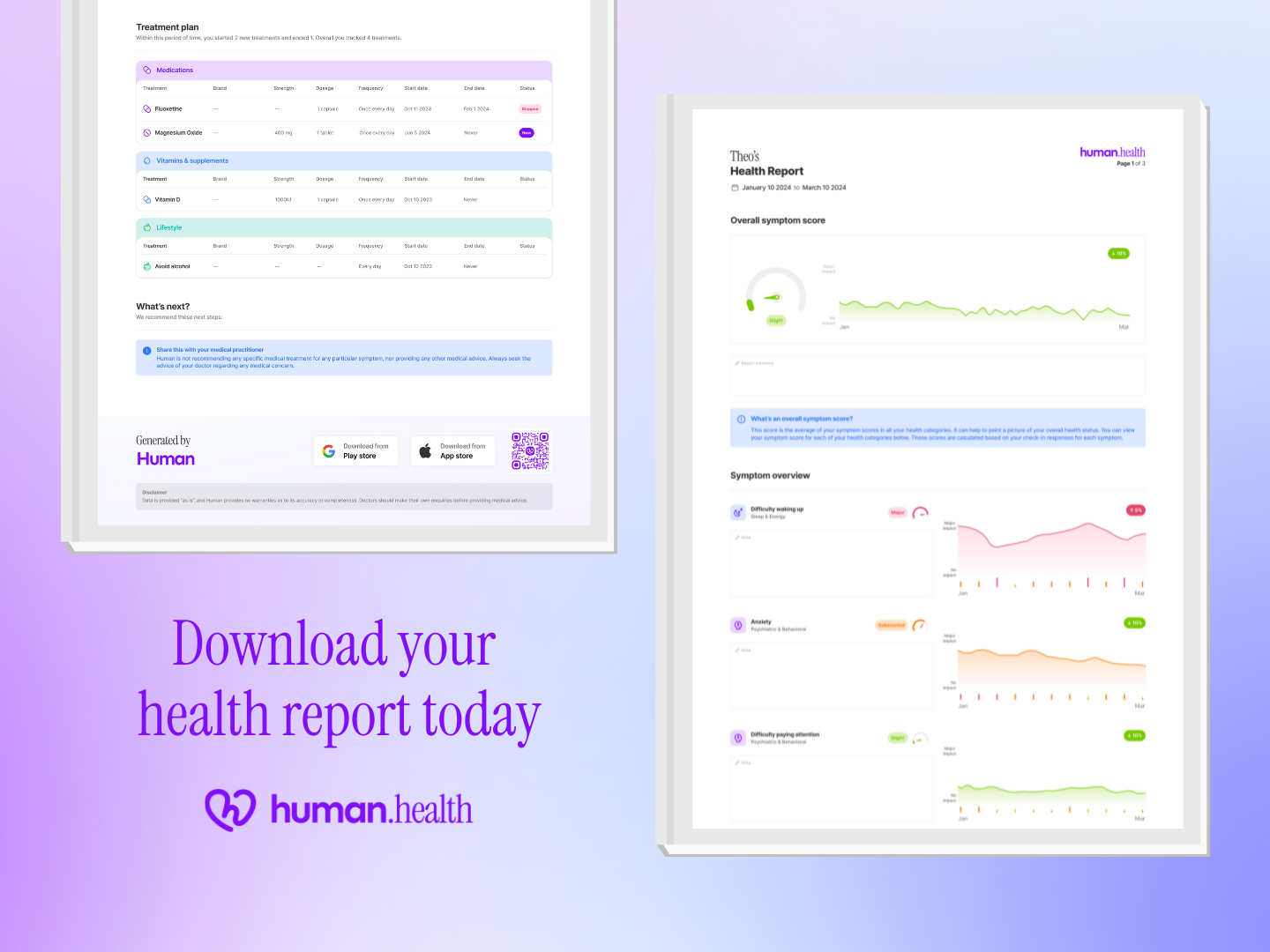
2. Use symptom tracking to support conversations
The Human Health app lets you track symptoms, daily habits, and experiences. You can export your information to share with your healthcare provider. Tracking is a way to organize what you notice, not to diagnose or manage a condition.
{{inline-cta-1}}
3. Be cautious with making sudden changes
There is limited information on how abrupt changes in nicotine use affect activity of the autonomic nervous system. If you are considering changes, it is important to discuss them with a doctor rather than acting on your own.
4. Consider other medications you take
If you use prescribed treatments, let your doctor know about smoking or vaping so they can consider this when reviewing your care plan.
#5: Keep support at the centre
Managing POTS often involves trial, observation, and adjustment. A supportive, ongoing relationship with your healthcare provider is key.
{{pro-tip-2}}
When to talk to your doctor
If symptoms change, worsen, or feel harder to manage, it is important to speak with a doctor. Only a healthcare provider can assess whether symptoms are related to POTS or another condition.
Worsening dizziness or fainting
If you notice dizziness becoming more frequent or more intense, or if you experience fainting or near-fainting episodes, this is a reason to contact your doctor. These symptoms can have many possible causes and should not be self-interpreted. Sharing when they occur, how often, and what was happening beforehand can help your healthcare provider decide what to check next.
Chest tightness or palpitations
Chest tightness, discomfort, or noticeable heartbeats can feel alarming. While these sensations do not automatically mean something serious, they should always be discussed with a doctor. Tracking when they happen, how long they last, and whether they occur at rest or after activity can lead to a clearer conversation with your doctor.
Fatigue that doesn’t improve
Ongoing fatigue that does not improve with rest or routine adjustments is another reason to seek medical advice. Fatigue can be linked to many health issues, not just POTS. A doctor can help determine whether further evaluation is needed and whether other factors should be considered.
Taken together, these symptoms are signals to seek medical advice rather than trying to interpret them on your own. A doctor can help assess what may be contributing and decide what steps, if any, are needed next.
Track POTS symptoms & flare-ups
If you are noticing symptoms and want a clearer picture to share with your doctor, tracking can be a helpful next step.
The Human Health app is designed for this. It lets you track symptoms, daily habits, and how you feel over time, all in one place.
By using the app consistently, you can build a clearer record of what’s happening in your body and feel better prepared for medical appointments.
{{inline-cta-2}}
References
Moheimani RS, Bhetraratana M, Yin F, Peters KM, Gornbein J, Araujo JA, Middlekauff HR. “Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: implications for cardiovascular risk” 2017; https://doi.org/10.1001/jamacardio.2016.5303
Lee MS. et al. “Cardiac autonomic effects of secondhand exposure to nicotine from electronic cigarettes” 2019; https://pmc.ncbi.nlm.nih.gov/articles/PMC6814191/
Garcia PD, Gornbein JA, Middlekauff HR. “Cardiovascular autonomic effects of electronic cigarette use: a systematic review”. Clin Auton Res. 2020; https://doi.org/10.1007/s10286-020-00683-4
Cohen DL, Townsend RR. “Does Cigarette Use Modify Blood Pressure Measurement or the Effectiveness of Blood Pressure Medications?” J Clin Hypertens (Greenwich). 2009; https://pmc.ncbi.nlm.nih.gov/articles/PMC8673017/
NHS. “Postural tachycardia syndrome (PoTS)”. NHS.uk. 2025. Available from: https://www.nhs.uk/conditions/postural-tachycardia-syndrome/
Bryarly M, Phillips LT, Fu Q, Vernino S, Levine BD. “Postural orthostatic tachycardia syndrome: JACC focus seminar”. J Am Coll Cardiol. 2019; https://doi.org/10.1016/j.jacc.2018.11.059
Disclaimer: The Human Health app is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with your healthcare provider.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

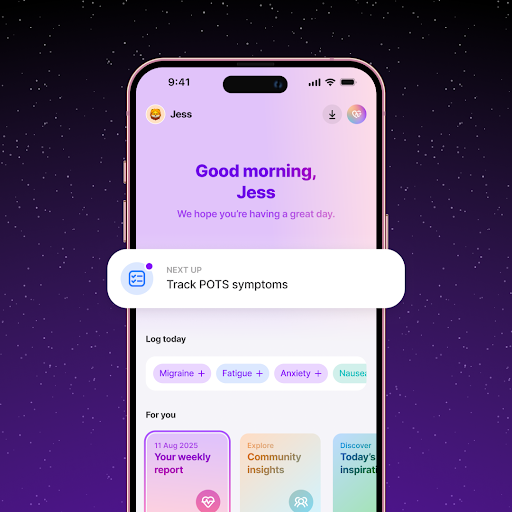
Using the Human Health App - Track How Smoking Affects Your POTS Symptoms
Log smoking habits alongside symptoms like dizziness, rapid heart rate, or fatigue to understand how smoking impacts your condition.
Share Insights with Your Healthcare Provider
Turn your smoking and symptom logs into clear reports using the Human Health app - that help your doctor give personalized advice and support.






Pro tip
Patterns can matter more than single bad days. Looking at patterns of symptom changes or flare-ups over several days or weeks can make it easier to explain what you are experiencing.
Pro tip
Bring notes, not assumptions, to appointments. Writing down symptoms, timing, and changes you have noticed (whether in the Human Health app or on paper) can help your doctor ask the right questions.

.jpg)




.png)

