Orthostatic Hypotension vs POTS: Similarities & Differences
October 1, 2025

- Orthostatic Hypotension (OH) and Postural Orthostatic Tachycardia Syndrome (POTS) are both conditions linked to changes in blood flow when standing.
- OH involves a significant drop in blood pressure, while POTS is defined by a rapid rise in heart rate without a major blood pressure drop.
- Both conditions may share symptoms like dizziness, fainting, or fatigue, but their root mechanisms differ.
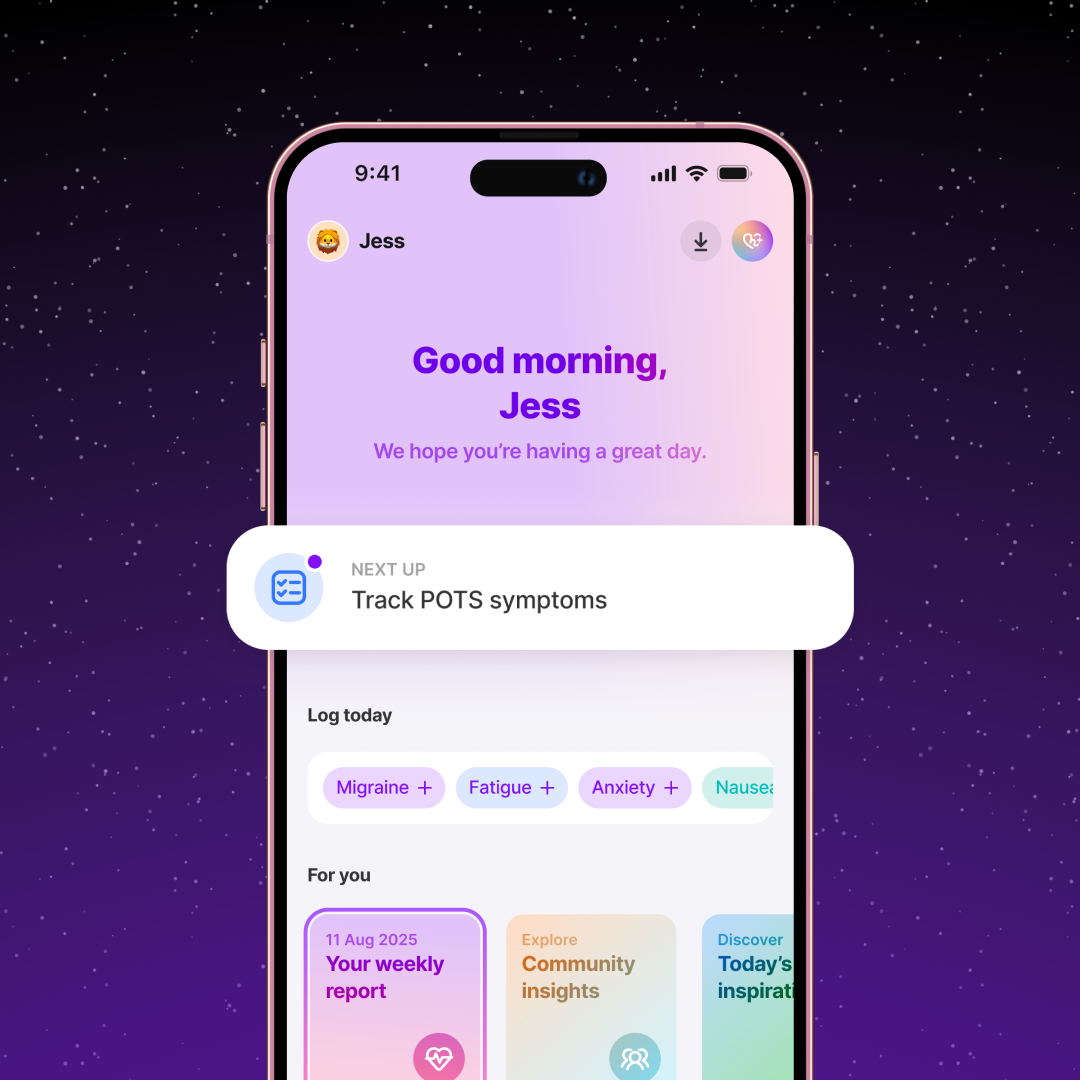
- Tracking symptoms, blood pressure, and heart rate with the Human Health app can help you and your provider identify patterns and discuss next steps.
Disclaimer: Human Health is a patient-led tracking platform and does not provide medical advice, diagnosis, or treatment. Always talk to a qualified healthcare provider about your symptoms and care options.
If you’ve ever stood up and felt your vision fade, your head spin, or your heart race so fast it scared you, you know how disruptive these symptoms can be.
Orthostatic hypotension (OH) and postural orthostatic tachycardia syndrome (POTS) are two conditions that often feel alike, but they differ in important ways. OH is driven by a sudden drop in blood pressure, while POTS is defined by a sharp rise in heart rate.
In this article, you’ll learn how to tell them apart, where they overlap, and how tracking your own symptoms can help bring clarity to your care.
The relationship between orthostatic hypotension and POTS
Orthostatic hypotension (OH) and Postural Orthostatic Tachycardia Syndrome (POTS) are both conditions that involve challenges with the body’s ability to regulate blood flow when moving from lying down or sitting to standing.
While OH is primarily defined by a significant drop in blood pressure when standing, POTS is characterized by a sustained rise in heart rate without a major blood pressure drop. Both fall under the umbrella of autonomic disorders, which is why people may experience overlapping symptoms like dizziness or fainting, making them sometimes difficult to distinguish.

Possible shared symptoms of POTS and orthostatic hypotension
Both POTS and orthostatic hypotension can affect how you feel when standing. Symptoms often overlap, which is why careful tracking and medical evaluation are so important. Using the Human Health app, you can log symptoms like dizziness, fainting, or fatigue and share patterns with your healthcare provider.
Dizziness and lightheadedness
Many people with either condition report dizziness or lightheadedness when standing up. This happens because the body struggles to adjust blood flow quickly enough, leading to reduced circulation to the brain.
Fainting (syncope)
Loss of consciousness (syncope) can occur in both POTS and OH, though it is less common in POTS. In OH, fainting often follows a sharp drop in blood pressure, while in POTS, it may result from an overworked cardiovascular system.
Fatigue and brain fog
Ongoing fatigue and difficulty concentrating (brain fog), are common in both conditions. These symptoms may stem from reduced blood flow to the brain and the body’s constant effort to maintain stability.
Palpitations
While palpitations are more strongly linked to POTS due to the rapid rise in heart rate, some people with OH also report palpitations among their symptoms.
Because these symptoms can look so similar, tracking how and when they occur gives you and your provider clearer insight into which condition might be driving them.
POTS vs. orthostatic hypotension: Differences
Although POTS and orthostatic hypotension share some symptoms, the way they affect blood pressure and heart rate sets them apart.
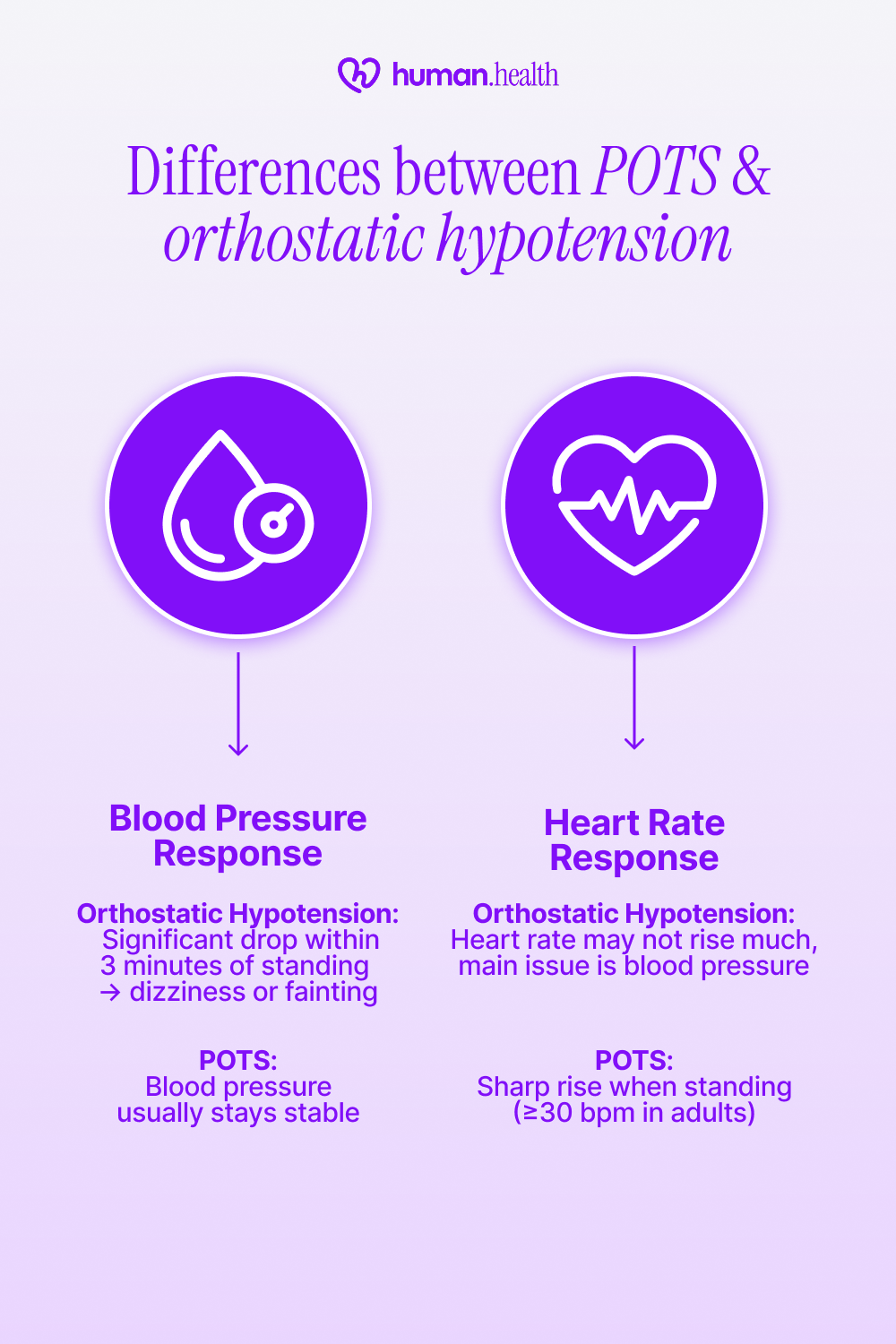
Blood pressure response
Orthostatic hypotension is defined by a significant drop in blood pressure (≥ 20 mmHg systolic or ≥ 10 mmHg diastolic) within 3 minutes of standing. This sudden dip can reduce blood flow to the brain, leading to dizziness or fainting. In contrast, people with POTS typically maintain stable blood pressure when upright.
Heart rate response
In POTS, standing up causes the heart rate to rise sharply (at least 30 beats per minute in adults), while there is no significant drop in blood pressure. This exaggerated response is a defining feature of the condition. With Oothostatic hypotension, the heart rate may not increase dramatically, since the primary issue lies in blood pressure regulation.
Focusing on how blood pressure and heart rate respond to standing is the clearest way to tell these two conditions apart.
With the Human Health app, you can log both blood pressure and heart rate changes when you stand. Over time, this information may reveal patterns worth sharing with your doctor.
How doctors diagnose orthostatic hypotension and POTS
Because the symptoms of POTS and orthostatic hypotension overlap, doctors rely on structured tests, vital sign measurements, and medical history to distinguish between the two. Delays or misdiagnoses are possible, which makes detailed symptom tracking even more valuable.
POTS
Doctors diagnose POTS when a patient experiences symptoms upon standing, along with a sustained heart rate increase of at least 30 beats per minute (in adults) within 10 minutes of standing, without a major blood pressure drop.
What the research shows
Research shows that a common diagnostic tool is the tilt-table test. In these studies, participants are monitored while moving from lying down to an upright position, with continuous tracking of blood pressure and heart rate.
- Sustained heart rate rise (≥30 bpm in adults, ≥40 bpm in adolescents)
- Symptoms triggered by upright posture (dizziness, palpitations, fatigue)
- No significant orthostatic blood pressure drop
Orthostatic Hypotension
Doctors diagnose orthostatic hypotension when systolic blood pressure falls by at least 20 mmHg, or diastolic blood pressure by at least 10 mmHg, within 3 minutes of standing.
What the research shows
Studies confirm that bedside blood pressure measurement after lying down, followed by standing readings, remains the gold standard.
- Drop in systolic BP ≥20 mmHg or diastolic BP ≥10 mmHg
- Symptoms like dizziness, lightheadedness, or fainting upon standing
- May require repeat testing at different times of day, since severity can vary
Structured testing and detailed records are the foundation of getting the right diagnosis, which is why your own logs can be so valuable in the process.
Managing orthostatic hypotension and POTS: Tips & advice
While only a healthcare provider can recommend treatments, many people explore lifestyle changes to help manage day-to-day symptoms.
#1: Track your symptoms
Use the Human Health app to log dizziness, fainting, heart rate, and blood pressure changes. Over time, this record may highlight triggers (like dehydration, stress, or fatigue) that you can discuss with your provider.
{{inline-cta-1}}
#2: Stay hydrated
Adequate fluid intake is often emphasized in medical literature for improving orthostatic tolerance and cardiovascular responses. People with POTS and OH may notice that dehydration makes symptoms worse.
#3: Compression garments
Some studies suggest that compression garments (like stockings or abdominal binders) can reduce blood pooling in POTS and some forms of orthostatic hypotension.
#4: Gentle movement
Slowly transitioning from lying down to standing, or doing light movement or exercise (especially from seated or supine positions), may help reduce sudden symptom spikes. Always check with your healthcare provider before starting new routines.
Small daily changes, paired with symptom tracking, may help you reduce flare-ups and feel more in control of both conditions.
You can explore more insights on POTS flare-up in our comprehensive guide.
Medications & treatment for orthostatic hypotension: What we know
Doctors sometimes prescribe medications when lifestyle strategies alone don’t provide enough relief. These approaches are studied carefully, as orthostatic hypotension can have multiple underlying causes.
What the research shows
Researchers have studied several medications for orthostatic hypotension, especially when lifestyle changes aren’t enough.
One randomized controlled trial published in JAMA (Low et al., 1997) found that midodrine significantly improved standing blood pressure and reduced lightheadedness in people with neurogenic OH.
A Cochrane review (2021) also found evidence for fludrocortisone, which works by expanding blood volume, though results were mixed and side effects like fluid retention were noted.
Another option, droxidopa, has shown benefits in clinical trials for improving blood pressure and symptoms, but there’s still limited data on long-term outcomes.
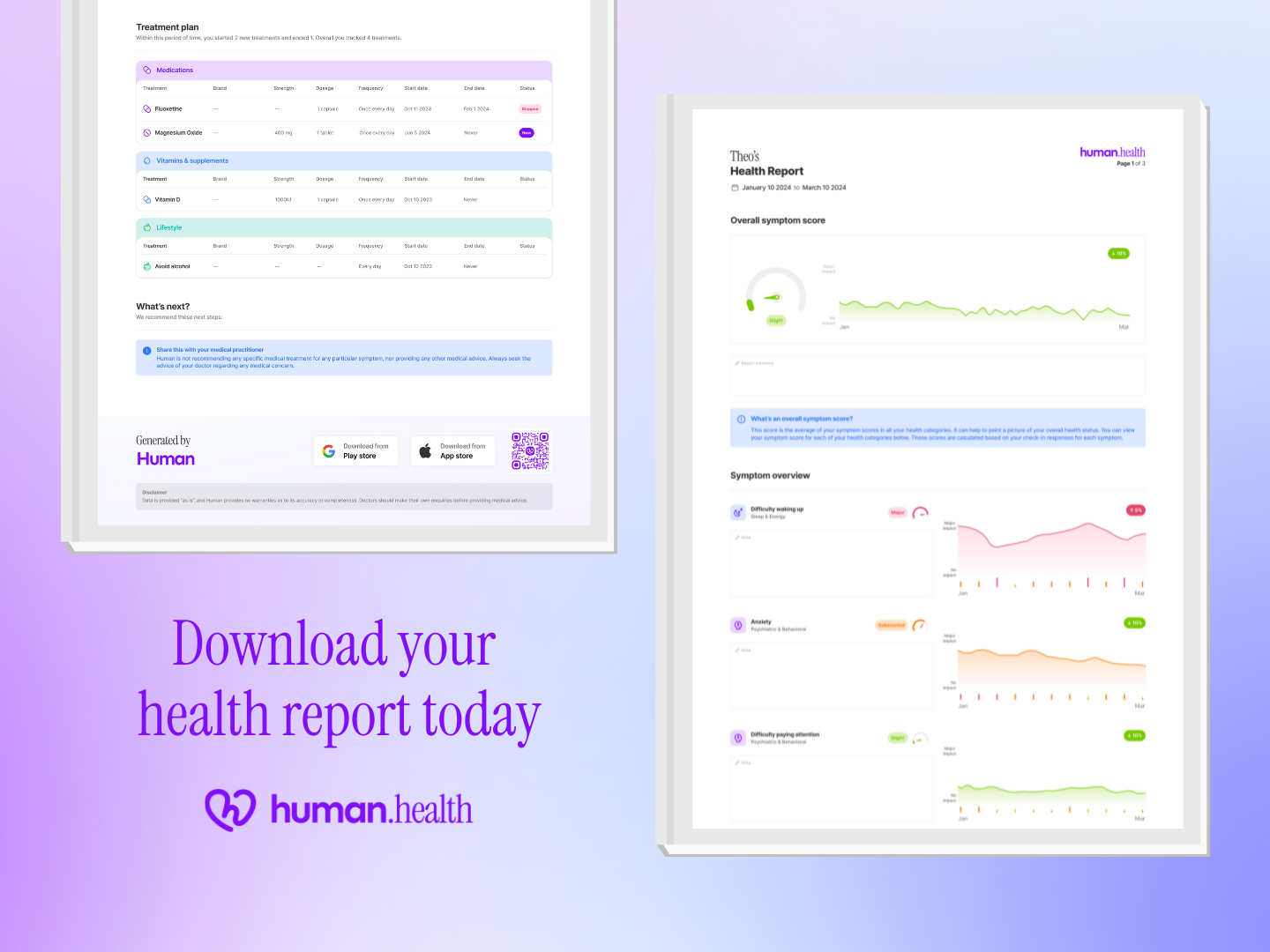
With the Human Health app, you can track which medications you are prescribed, note any side effects, and share this information with your healthcare provider to help tailor your care plan.
How doctors treat POTS today
Postural Orthostatic Tachycardia Syndrome (POTS) is managed with a combination of lifestyle adjustments and, in some cases, medications when symptoms significantly impact quality of life.
What the research shows
Studies have looked at different medications to help manage POTS symptoms when lifestyle strategies aren’t enough.
In randomized trials, low-dose propranolol was shown to ease tachycardia and improve symptoms for some people, though not everyone responds the same way.
A 2021 randomized controlled trial also found that ivabradine, a medication that slows heart rate without lowering blood pressure, reduced standing heart rate and improved quality of life in patients with hyperadrenergic POTS.
Other medications, like fludrocortisone or pyridostigmine, have also been studied, but results are mixed, and side effects can be a concern. Because of this, researchers emphasize that no single treatment works for everyone, and management often needs to be tailored to each person.
If you’d like to discover practical ways to manage symptoms, we’ve compiled a list of Natural Remedies for POTS in our detailed blog post.
Use the Human Health app to track symptoms, flares, patterns & more
Living with orthostatic hypotension or POTS can feel unpredictable, but keeping track of your health doesn’t have to be overwhelming. With the Human Health app, you can log daily symptoms, blood pressure, and heart rate, then export practitioner-ready PDF summaries for your appointments.
By spotting patterns and bringing clear reports to your provider, you’ll feel more prepared for check-ups, more confident in your care, and less weighed down by the uncertainty these conditions can bring.
Start tracking with Human Health today and take the first step toward making your health journey feel more manageable.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
References
- National Library of Medicine: Orthostatic Hypotension
- National Institute of Neurological Disorders and Stroke: Postural Tachycardia Syndrome (POTS)
- National Library of Medicine: Differential diagnosis of orthostatic hypotension
- National Library of Medicine: Orthostatic Hypotension: Management of a Complex, but Common, Medical Problem
- National Library of Medicine: Diagnosis and treatment of orthostatic hypotension
- The Journal for Nurse Practitioners: Postural Orthostatic Tachycardia Syndrome (POTS): A Frequently Missed Diagnosis
- National Library of Medicine: Postural Orthostatic Tachycardia Syndrome
- National Library of Medicine: Evaluation and management of orthostatic hypotension
- Johns Hopkins Medicine: Postural Orthostatic Tachycardia Syndrome (POTS)
- National Library of Medicine: Diagnosis and management of postural orthostatic tachycardia syndrome
- National Library of Medicine: Abdominal Compression as a Treatment for Postural Tachycardia Syndrome
- National Library of Medicine: Preventing and treating orthostatic hypotension: As easy as A, B, C
- National Library of Medicine: Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. A randomized, double-blind multicenter study. Midodrine Study Group
- Cochrane: Fludrocortisone for the treatment of orthostatic hypotension
- BMC Neurology: Integrated analysis of droxidopa trials for neurogenic orthostatic hypotension
- National Library of Medicine: Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: less is more
- National Library of Medicine: Randomized Trial of Ivabradine in Patients With Hyperadrenergic Postural Orthostatic Tachycardia Syndrome
- Autonomic Neuroscience: Pharmacotherapy for postural tachycardia syndrome
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

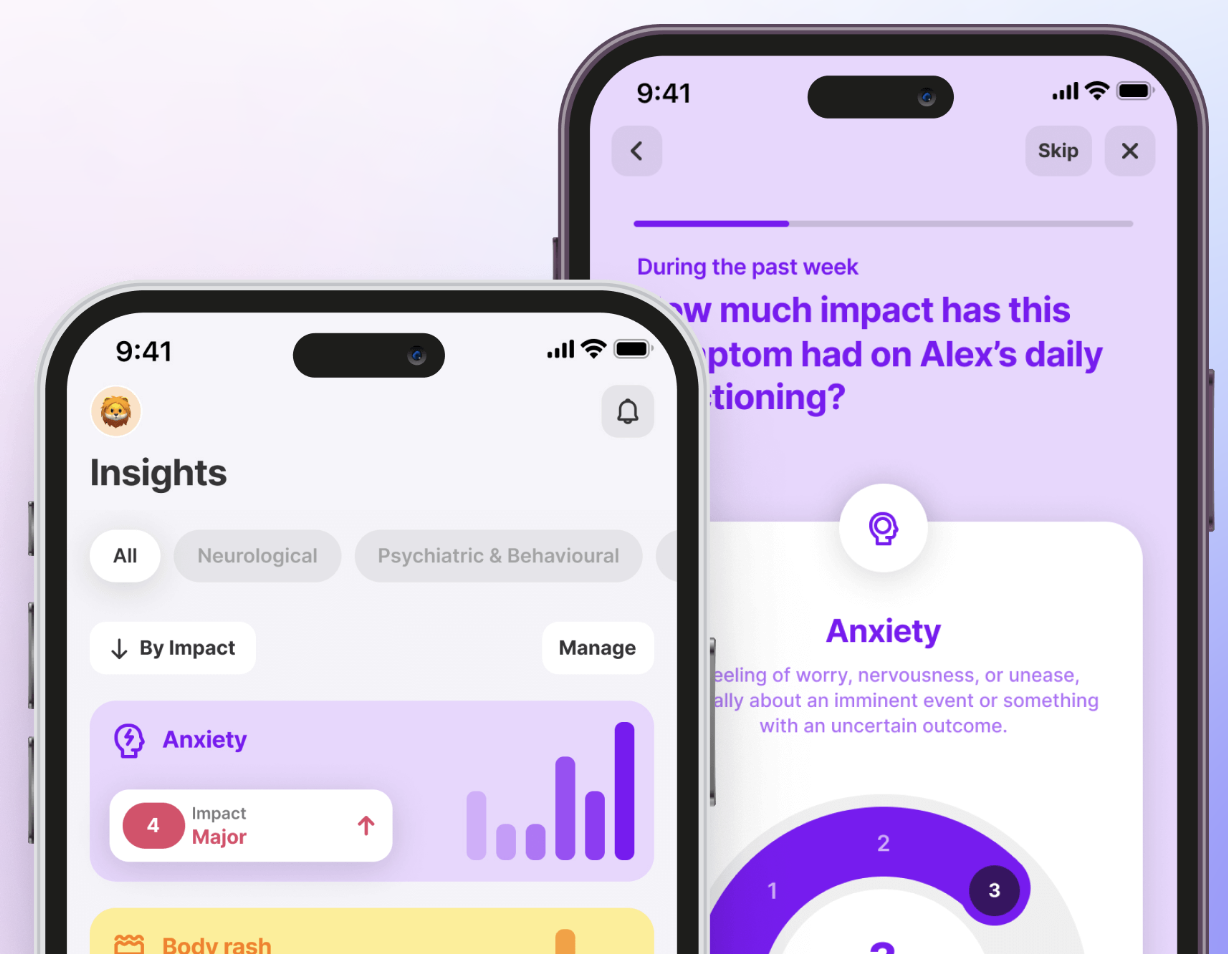
Track All Your Symptoms with the Human Health App
Spot patterns in your symptoms, capture the frequency, and the type of symptoms, without having to rely on memory.








.jpg)




.png)

