POTS and Blood Sugar: Connection & Management Tips
November 5, 2025

- POTS (Postural Orthostatic Tachycardia Syndrome) may influence blood sugar regulation because of how it affects the autonomic nervous system, which controls involuntary body processes.
- People with POTS can experience symptoms similar to blood sugar dips, like dizziness, fatigue, or shakiness, especially after meals.
- Managing blood sugar levels through balanced meals, hydration, and consistent tracking can help stabilize energy and reduce symptom flare-ups.
- Using tools like the Human Health app to log symptoms and triggers makes it easier to see patterns and share accurate data with healthcare providers.
Disclaimer: This article is for information only. Human Health does not provide medical advice, diagnosis, or treatment. Always talk to a qualified healthcare provider about your health.
If you live with POTS (Postural Orthostatic Tachycardia Syndrome), you may have noticed that certain meals (or going too long without food) seem to make you feel dizzy, shaky, or unusually tired.
You’re not alone in noticing that pattern.
Some people with POTS report that changes in blood sugar may influence their symptoms, although research on this connection is still emerging.
Because POTS affects how the autonomic nervous system regulates heart rate, blood flow, and digestion, these same systems can also play a role in blood sugar balance. When they don’t work in sync, symptoms can appear that feel similar to blood sugar spikes or crashes.
In this article, you’ll explore what scientists currently understand about the link between POTS and blood sugar, the shared symptoms, and practical ways to monitor these patterns so you can feel steadier throughout your day.
The connection between POTS and blood sugar
While research is still developing, several studies suggest that autonomic dysfunction (the same process that drives POTS symptoms) may also affect how your body regulates glucose. The autonomic nervous system helps control heart rate, blood pressure, and digestion, but it also plays a key role in how insulin and other hormones manage blood sugar. When these signals are disrupted, it may lead to fluctuations that resemble low or high blood sugar episodes.
Does POTS possibly affect blood sugar?
It might. Some evidence indicates that POTS may influence how the body manages glucose, particularly after meals. Because the autonomic nervous system helps control blood flow to the digestive tract and pancreas, disrupted signaling could alter insulin release or digestion. This may explain why some people with POTS feel lightheaded or fatigued after eating, even when their blood sugar readings look normal.
Could POTS be related to diabetes?
Not directly, but there may be overlap. POTS doesn’t cause diabetes, and diabetes doesn’t cause POTS. However, both can involve autonomic nervous system changes that affect how the body handles glucose. Some symptoms (like dizziness, fatigue, or a rapid heartbeat after meals) can appear in both conditions, which is why medical testing is needed to tell them apart.
Tracking these reactions over time can help you and your healthcare provider identify patterns and develop more personalized strategies for stability.
Learn how POTS and PCOS overlap.
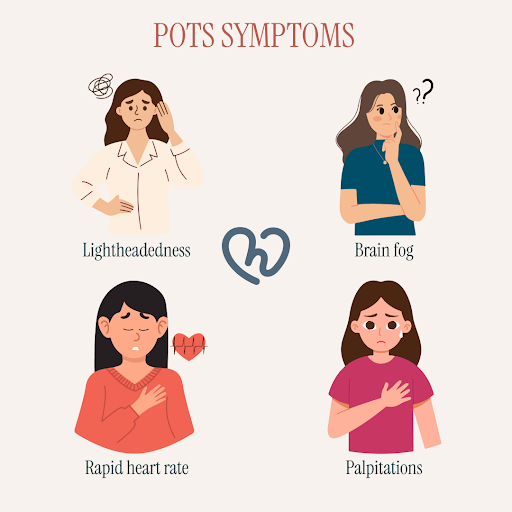
Shared symptoms of blood sugar fluctuations & POTS
Because both POTS and blood-sugar changes affect circulation and energy balance, their symptoms can overlap. You might notice several of these sensations, especially after eating or standing for long periods.
1. Dizziness and lightheadedness
Feeling dizzy or faint is one of the most common POTS symptoms. Standing can cause blood to pool in the lower body, which reduces blood flow to the brain and leads to lightheadedness. When this happens after eating, it may feel similar to a blood-sugar drop and leave you unsteady or off balance.
2. Shakiness or trembling
When blood sugar falls, the body releases adrenaline to restore balance. That same adrenaline response can make POTS symptoms stronger, causing trembling, a faster heartbeat, or feelings of anxiety
3. Fatigue after meals
Feeling tired or needing to rest after eating may be linked to how the body redirects blood to the digestive system. Some studies suggest that glucose intake can temporarily increase heart rate in people with POTS, which might explain the wave of fatigue that follows larger meals.
4. Rapid heartbeat
Both blood-sugar changes and POTS can raise heart rate. When glucose levels shift quickly, stress hormones rise and may further speed up the heartbeat, adding to the circulatory changes already present in POTS.
5. Nausea or stomach discomfort
The autonomic nervous system helps control digestion, and in POTS it may not always function smoothly. This can slow stomach emptying and cause nausea or fullness after meals. When combined with blood-sugar changes, these effects can make eating feel uncomfortable.
Noting when these sensations occur (after eating, standing, or during stress) can help your healthcare provider understand patterns and guide next steps.
How POTS might affect blood sugar
The autonomic nervous system (ANS) plays a key role in both circulation and metabolism. It helps regulate heart rate, blood pressure, and hormone release (including insulin and glucagon, which control blood sugar). In POTS, where autonomic control is disrupted, these systems may not communicate smoothly. That can make blood-sugar responses less predictable, especially after eating or during stress.
1. Autonomic dysfunction and glucose control
The ANS helps manage when the body releases insulin and glucagon. The sympathetic nerves can lower insulin and raise glucagon, while the parasympathetic nerves encourage insulin release. When this signaling doesn’t work properly, blood-sugar levels can swing up or down more easily. This might explain why some people with POTS feel weak, shaky, or dizzy even when glucose readings look normal.
Learn more about whether POTS may have a genetic connection.
2. Hormone imbalances
People with POTS may also experience changes in stress hormones that affect metabolism. Cortisol and adrenaline can fluctuate more than usual, with higher cortisol levels sometimes raising blood sugar, and sudden spikes in adrenaline causing sharper drops. These shifts may add to fatigue or lightheadedness, particularly around mealtimes.
3. Reactive hypoglycemia
Some studies suggest that people with POTS can develop reactive hypoglycemia, a temporary drop in blood sugar, a few hours after eating. In one observational study, about 40% of participants with POTS showed low glucose levels several hours into a glucose test. These dips may trigger tiredness, palpitations, or dizziness similar to a POTS flare. Eating smaller, balanced meals may help reduce these fluctuations, but any changes should be discussed with a healthcare provider.
While not everyone with POTS experiences these changes, tracking meals, symptoms, and timing can help uncover patterns to discuss with your healthcare provider.
{{inline-cta-1}}
Practical tips for managing blood sugar fluctuations & POTS
Managing both POTS and blood sugar swings often comes down to small, consistent habits. These strategies can help keep your energy levels steadier and minimize post-meal crashes.
1. Eat smaller, balanced meals
Large meals can worsen POTS symptoms because digestion redirects a significant amount of blood to the gut, causing more pooling and reduced circulation elsewhere. Try smaller, frequent meals with a mix of protein, fiber, and healthy fats to support gradual blood sugar release and reduce fatigue after eating.
Top Tip: Start your day with balance.
Try pairing a source of protein (like eggs, yogurt, or nut butter) with slow-release carbohydrates at breakfast. This may help maintain steadier blood sugar levels through the morning and reduce early-day lightheadedness or fatigue.
2. Focus on low-glycemic foods
Choose low-glycemic foods (such as oats, quinoa, lentils, leafy greens) that release glucose more steadily, helping prevent sudden rises and crashes in blood sugar that may trigger dizziness or brain fog.
3. Stay hydrated and add electrolytes
Adequate hydration plays a key role in POTS management. Drinking water regularly and using electrolyte solutions that are low in added sugar can help maintain blood volume and support circulation. This, in turn, may lessen tachycardia and pooling, two common POTS-related challenges.
4. Limit added sugars and processed carbs
Highly processed or sugary foods can trigger quick blood-sugar rises followed by sharp drops. For people with POTS, these swings may intensify feelings of shakiness, weakness, or fatigue. Replacing them with whole foods (like fruit, vegetables, and complex carbohydrates) can help maintain steadier energy.
5. Track symptoms and triggers
Keeping a record of what you eat, how you feel afterward, and when symptoms appear can uncover helpful patterns over time.
Take control of your daily data - start logging your meals and symptoms with the Human Health app today to better understand what triggers your POTS flares.
Try these natural POTS relief tips to feel more steady.
Could POTS possibly be misdiagnosed as blood sugar problems?
It can happen, since several symptoms of POTS (like dizziness, palpitations, and faintness) are similar to those caused by changes in blood sugar. This overlap can make the two conditions difficult to tell apart at first. Some people may initially suspect a blood-sugar issue before discovering that their symptoms are linked to autonomic dysfunction instead.
Because both conditions affect circulation and energy balance, even healthcare providers may need time and detailed testing to separate them. Tracking when symptoms occur (for example, after standing up, eating, or resting) can help provide important clues.
Keeping consistent records through tools like the Human Health app gives your healthcare provider a clearer timeline. Tests such as tilt-table assessments or glucose tolerance testing can then be interpreted with more context, leading to more accurate results and a care plan tailored to your needs.

Does treating blood sugar issues help with POTS?
Keeping blood sugar more stable may help ease some symptoms that overlap with POTS. When glucose levels stay consistent, the body experiences fewer sharp changes in heart rate, blood pressure, or energy. All of which can contribute to a steadier day.
Simple habits like eating balanced meals at regular intervals, staying hydrated, and limiting high-sugar or highly processed foods can support this stability. These approaches won’t treat POTS itself but may help minimize symptom flare-ups related to post-meal fatigue or dizziness.
If you suspect that blood-sugar fluctuations are making your POTS symptoms worse, it’s important to discuss this with a healthcare provider. They can recommend appropriate testing, such as glucose tolerance assessments, or refer you to a specialist who can look for related issues like reactive hypoglycemia or insulin resistance.
Top Tip: Track before you tweak.
Before changing your meals or routines, log your current habits for a week. Seeing how food, hydration, and activity affect your symptoms makes it easier to identify what truly helps and gives your healthcare provider clearer data to work with.
Manage all your conditions with the Human Health app
Living with POTS and blood-sugar changes can feel unpredictable. Tracking everything manually can be overwhelming, but you do not have to do it alone.
With the Human Health app, you can log your symptoms, meals, and routines in one secure place and start uncovering real patterns. These insights help you see what supports your energy and what may trigger flares, making every conversation with your healthcare provider more productive.
You can also export organized health summaries to share before appointments, giving your care team the context they need to personalize your plan.
Download the Human Health app and begin tracking what matters most to you. Each entry brings you closer to clarity, confidence, and better-informed care.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site supports, not replaces, conversations with qualified healthcare professionals.
References
- National Library of Medicine: Heart Rate, Autonomic Function, and Future Changes in Glucose Metabolism in Individuals Without Diabetes: The Whitehall II Cohort Study
- ScienceDirect: Metabolic targets in the Postural Orthostatic Tachycardia Syndrome: A short thematic review
- Metabolism - Clinical and Experimental: Association of Fasting Blood Glucose Levels in Patients with Postural Orthostatic Tachycardia Syndrome (POTS): A Study Stratified by Age Groups
- Endocrine Abstracts: A retrospective observational-cohort study of the relationship between reactive hypoglycaemia to postural orthostatic tachycardia syndrome (PoTS)
- National Library of Medicine: Adrenaline: insights into its metabolic roles in hypoglycaemia and diabetes
- National Library of Medicine: Worsening Postural Tachycardia Syndrome is Associated with Increased Glucose Dependent Insulinotropic Polypeptide Secretion
- National Library of Medicine: Gastric Emptying in Postural Tachycardia Syndrome: A Preliminary Report
- Johns Hopkins Medicine: Postural Orthostatic Tachycardia Syndrome (POTS)
- Nature: Autonomic control of energy balance and glucose homeostasis
- National Library of Medicine: Peripheral innervation in the regulation of glucose homeostasis
- Cleveland Clinic: Postural Orthostatic Tachycardia Syndrome (POTS)
- UF Food Science & Human Nutrition: Navigating Life with POTS: A Journey of Discovery and Nutrition
- National Library of Medicine: Diagnosis and management of postural orthostatic tachycardia syndrome: A brief review
- Journal of UOEH: A Case of Postural Orthostatic Tachycardia Syndrome (POTS) with Difficulties in Differentiation from Hypoglycemic Attack
- Standing Up to POTS: Nutritional Strategies to Help Manage POTS
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Track your blood sugar and POTS symptoms together with the Human Health app
Log blood sugar levels, dizziness, fatigue, and meal times to see how your glucose patterns affect POTS symptoms throughout the day.








.jpg)




.png)

