8 Tips for Fibromyalgia Stress Management in 2026
January 15, 2026
- Fibromyalgia and stress are closely connected. Stress is described as a possible trigger for symptoms and may affect how strong symptoms feel for some people.
- Fibromyalgia involves changes in how the brain and spinal cord process pain. Stress response systems in the body are thought to play a role, but study results are not always the same.
- Emotional health is an important part of fibromyalgia. Depression and anxiety are reported in many people with the condition and are linked to a higher overall burden.
- Noticing patterns between stress, sleep, mood, and pain can help you explain your experience more clearly to a healthcare provider. Only a doctor can diagnose fibromyalgia or related conditions.
Disclaimer: This guide is for informational purposes only. It is not medical advice and should not be used to diagnose, treat, or manage any condition. Always speak with a doctor or qualified healthcare provider about any symptoms or health concerns.
Fibromyalgia and stress are closely linked, and many people living with fibromyalgia notice that stressful periods can change how their symptoms feel.
If you searched for the connection between fibromyalgia and stress, the short answer is that stress is often described as a factor that may influence symptom intensity.
In this guide, you will find a clear explanation of that link, what research suggests, and how to better understand your own patterns before discussing them with a doctor.
The connection between fibromyalgia and stress
Fibromyalgia and stress are closely linked. Some people report that stress is present before symptoms begin or during symptom flare-ups. Emerging evidence suggests that stress may influence how the body processes pain and how intense symptoms feel.
Research also describes stress as a factor linked to poorer outcomes and a higher overall burden for people living with fibromyalgia. However, these effects can vary widely from person to person, and no single cause has been confirmed.
The possible effect of stress on fibromyalgia
Stress may affect fibromyalgia in several different ways. Research findings are mixed, and not everyone experiences these effects in the same way.
Changes in pain processing
Fibromyalgia is linked to changes in how the brain and spinal cord handle pain signals. Some studies suggest stress response systems in the body may be involved in this process, which could make pain feel stronger for some people. Evidence is not consistent across all studies.
Increased emotional strain
Depression and anxiety are reported in many people with fibromyalgia. Ongoing stress may add to emotional strain, which is associated with a higher overall symptom burden.
Sleep disruption
Sleep problems are common in fibromyalgia. Research notes that stress and poor sleep often occur together. Disrupted sleep is associated with increased pain, while pain itself may further disturb sleep, creating a difficult cycle for some people.
{{pro-tip-1}}
8 tips to manage fibromyalgia-related stress
People experience fibromyalgia-related stress in different ways. The tips below reflect patterns described in research and patient reports. Effects can vary, and these are not medical treatments.
Tip 1: Learn more about fibromyalgia and stress
Some people report that understanding fibromyalgia helps them make sense of their symptoms. Clinical guidelines suggest that patient education is a core part of care. Knowing that stress may influence symptoms can support clearer discussions with a healthcare provider.
Tip 2: Notice emotional health changes
Studies report that anxiety and depression are common in people with fibromyalgia. Some people notice emotional strain during periods of higher stress. Paying attention to mood changes may help you describe your experience more clearly to a doctor.
Tip 3: Track stress, sleep, and pain together
Fibromyalgia symptoms can fluctuate, and stress and sleep changes may influence how pain feels from day to day. Keeping simple notes on stress levels, sleep quality, and pain intensity can help you see whether changes tend to happen at the same time. This kind of record can also make it easier to explain your symptom patterns to a healthcare provider.
{{inline-cta-1}}
Tip 4: Be aware of physical stressors
Studies describe physical stress, such as injury or trauma, as possible triggers for fibromyalgia symptoms in some cases. Noting physical strain or major events alongside symptoms may add helpful context during medical visits.
Tip 5: Notice cognitive or focus changes
Cognitive difficulties are commonly reported in fibromyalgia. Some people notice changes in focus or clarity during times of high stress. Observing when these changes happen may help you explain your symptoms more fully.
Tip 6: Watch for symptom clustering
Fibromyalgia has multiple symptoms, including pain, fatigue, sleep issues, and emotional distress. Some people report these symptoms increasing together during stressful periods. Tracking clusters may reveal useful patterns.
Tip 7: Prepare information for appointments
Because stress may influence several symptoms at once, having notes can be helpful. Writing down stressors, emotional changes, sleep issues, and pain levels may support more focused conversations with a doctor.
Tip 8: Recognize when stress feels overwhelming
Some people notice that ongoing stress feels harder to cope with over time. Recognizing this may signal the need to speak with a healthcare provider.
{{pro-tip-2}}
When to consult a doctor for fibromyalgia-related stress
It may be time to consult a doctor if stress feels constant, overwhelming, or starts to coincide with changes in pain, sleep, mood, or daily functioning.
A doctor can help assess what is happening and discuss next steps. You may also find it helpful to read about patient experiences with therapy recommendations.

Track fibromyalgia symptoms and treatments with the Human Health app
Stress does not affect fibromyalgia the same way for everyone, and research findings are not always consistent. What often helps is understanding your own patterns, especially how stress, sleep, mood, and pain seem to overlap across weeks or months.
The Human Health app can help you capture those changes in a simple timeline, so you have clearer details to bring to your healthcare provider.
If you want a practical starting point, download the Human Health app and begin tracking at your own pace.
{{inline-cta-2}}
References
Beiner E, Victoria Lucas V et al. “Stress biomarkers in individuals with fibromyalgia syndrome: a systematic review with meta-analysis” 2023; https://pubmed.ncbi.nlm.nih.gov/36728497/
Galvez-Sánchez CM, Montoro CI “Psychoeducation for Fibromyalgia Syndrome: A Systematic Review of Emotional, Clinical and Functional Related-Outcomes” 2023; https://pmc.ncbi.nlm.nih.gov/articles/PMC10215575/
Jones EA, Asaad F et al. “Management of Fibromyalgia: An Update” 2024; https://pmc.ncbi.nlm.nih.gov/articles/PMC11201510/
Bhargava J, Goldin J “Fibromyalgia” 2025; https://www.ncbi.nlm.nih.gov/books/NBK540974/
Disclaimer: The Human Health app is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with your healthcare provider.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

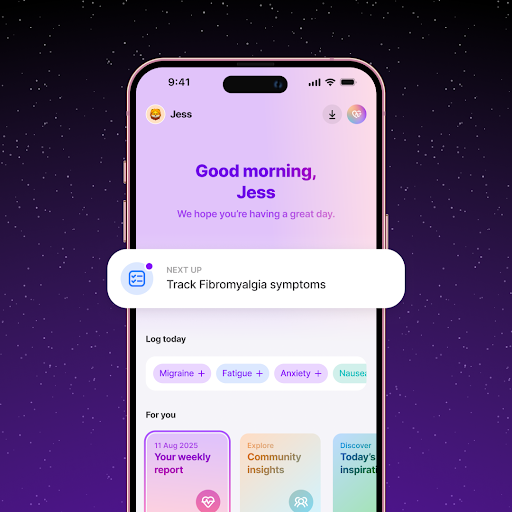
Track Stress and Fibromyalgia Symptoms with the Human Health app
Log daily stress levels alongside pain, fatigue, and sleep to see how stress affects your fibromyalgia flare-ups.
Share Stress Insights with Your Care Team
Use the Human Health app to stay consistent with stress-management habits and understand how routine supports symptom control.






Pro tip
The Human Health app lets you track symptoms, daily habits, and experiences. Tracking patterns between stress and symptoms may help you share clearer information with your healthcare provider.
Pro tip
Focus on one stress lever at a time. Instead of trying to fix sleep, mood, and pain all at once, choose one area to watch for two weeks and see what changes. This can make patterns easier to spot and less overwhelming to explain to a healthcare provider.

.jpg)





.png)

