Differences Between Fibromyalgia and Chronic Fatigue Syndrome
January 20, 2026

- Fibromyalgia and chronic fatigue syndrome are different conditions, even though they can feel similar to live with.
- Fibromyalgia is commonly characterized as ongoing, widespread pain, while chronic fatigue syndrome describes persistent, overwhelming fatigue that does not improve with rest.
- Some experiences can overlap. People may report fatigue, pain, sleep problems, and difficulties with concentration in both conditions.
- Symptoms can look alike, so diagnosis relies on medical assessment and careful exclusion of other causes. Only a doctor can tell the difference.
Disclaimer: This guide is for informational purposes only. It is not medical advice and should not be used to diagnose, treat, or manage any condition. Always speak with a doctor or qualified healthcare provider about any symptoms or health concerns.
Ongoing pain or exhaustion can be hard to make sense of, particularly when symptoms shift or overlap.
Although fibromyalgia and chronic fatigue syndrome are often talked about together, they’re defined by different core symptoms.
This guide explains how they differ, where they overlap, and how each can affect daily life.
What’s the difference between fibromyalgia and chronic fatigue syndrome?
The main difference is whether ongoing pain or overwhelming fatigue is the dominant issue. The sections below explain how they usually differ.
Fibromyalgia symptoms
People describe fibromyalgia as being mainly centred around pain. Experiences may vary from person to person.
- Widespread pain
Pain is often felt across multiple areas of the body and can be present most days. - Sensitivity
Some people notice increased sensitivity to touch, pressure, temperature, or noise. - Fatigue and sleep problems
Tiredness and unrefreshing sleep may occur, even after spending enough time in bed. - Cognitive difficulties
Problems with focus or memory are sometimes reported.
Symptoms can change over time and may not follow a clear pattern.
Chronic fatigue syndrome symptoms
Chronic fatigue syndrome is mainly defined by ongoing exhaustion that affects daily functioning.
- Persistent fatigue
Fatigue is usually severe, lasts for months, and is not relieved by rest. - Post-exertional symptom worsening
Physical or mental effort may lead to a noticeable increase in symptoms afterward. - Reduced stamina
Everyday tasks may feel much harder than before. - Cognitive and sleep changes
Concentration issues and sleep problems are commonly reported.
Only a doctor can assess symptoms and determine whether they fit chronic fatigue syndrome or another condition.

Possible overlapping symptoms between the two
Fibromyalgia and chronic fatigue syndrome are separate conditions, but some experiences may overlap. This overlap can make it harder to understand what is driving symptoms without medical input.
1. Fatigue
People with either condition may experience ongoing tiredness. This fatigue may feel disproportionate to activity levels and may interfere with work, social life, or daily routines.
2. Sleep problems
Sleep may feel unrefreshing in both conditions. Some people report difficulty falling asleep, staying asleep, or waking up feeling rested, even after enough time in bed.
3. Cognitive difficulties
Problems with concentration, memory, or mental clarity may occur. These experiences are often described as feeling mentally slowed or having trouble focusing on tasks or conversations.
{{pro-tip-1}}
What may be causing these conditions?
The exact causes of fibromyalgia and chronic fatigue syndrome are not fully understood. Doctors may look at patterns, triggers, and life events to better understand what might be contributing in each person.
Physical or emotional stress
Some people report that symptoms began or changed after periods of high stress. Stress may be a trigger, but it is not considered a direct cause.
Infections or illness
Symptoms may appear after an infection or a prolonged illness. This does not mean that infections cause these conditions; it only means that the timing may overlap.
Sleep disruption
Ongoing sleep problems are commonly reported. Poor sleep quality might be linked to how symptoms are experienced day to day.
Changes in daily activity levels
Large shifts in physical or mental activity may coincide with changes in symptoms. Noticing patterns around activity can sometimes provide useful context for discussions with a doctor.
Individual sensitivity and biology
Responses to pain, fatigue, or exertion may differ from person to person. These differences are still under study and are not fully understood.
The Human Health app lets you track symptoms, daily habits, and experiences, so you can notice possible patterns and export your information to share with your healthcare provider.
{{inline-cta-1}}
How fibromyalgia and chronic fatigue syndrome affect daily life
Living with fibromyalgia or chronic fatigue syndrome can influence many parts of everyday life. Experiences vary, and symptoms may change over time.
- Daily activities
Tasks like work, household chores, or social plans may feel harder to manage, especially on days when symptoms are more noticeable. - Energy and pacing
People may need to adjust how they plan their day due to limited or unpredictable energy levels. - Cognitive demands
Concentration, memory, or mental clarity may affect productivity and decision-making. - Emotional and social impact
Ongoing symptoms can affect mood, relationships, and participation in social activities.
{{pro-tip-2}}
What are the possible treatments and management available?
There is no single approach that works for everyone. Doctors may suggest different treatment options based on symptoms, medical history, and individual needs.
1. Medical evaluation and monitoring
A doctor may focus on careful assessment over time. This can include monitoring symptoms, ruling out other conditions, and adjusting care plans as new information emerges.
2. Symptom-focused discussions
Some care plans focus on addressing the most disruptive symptoms first, such as pain, fatigue, or sleep issues. Any decisions are made between you and your healthcare provider.
3. Lifestyle and daily adjustments
Doctors may discuss daily routines, activity levels, or sleep habits. These conversations aim to understand how everyday factors relate to symptom patterns, not to prescribe solutions.
4. Mental and emotional support
Living with long-term symptoms can be emotionally challenging. Some people are offered support options like therapy to help them cope with stress or the impact on daily life.
5. Tracking symptoms and patterns
Tracking can support medical conversations by showing patterns over time. The Human Health app helps you record symptoms, flare-ups, test results, and treatments in one place, then export a clear summary to share with your healthcare provider.
Management often involves observation, discussion, and adjustment over time rather than a single solution. Working with a doctor and bringing clear information about your symptoms can help guide those decisions and support more informed care.
When to talk to a doctor
It may be helpful to speak with a doctor if symptoms are ongoing, unexplained, or affecting daily life. Only a doctor can assess symptoms and determine what may be happening.
- Symptoms such as pain or fatigue last for months
- Daily activities become harder to manage
- Symptoms change, worsen, or appear suddenly
- You are unsure what might be causing your symptoms
{{pro-tip-3}}
Track your fibromyalgia and fatigue symptoms
Living with long-term pain or fatigue often means carrying a lot of uncertainty. When symptoms change or overlap, it can be difficult to feel confident explaining what you’re experiencing or deciding what to focus on next.
Using the Human Health app gives you a practical way to stay organised, build a clearer picture over time, and feel more prepared when you speak with your healthcare provider. It’s a small, steady step that can make managing ongoing symptoms feel more manageable.
If you want a structured way to start, explore the Chronic Illness Symptom Tracker to begin recording your symptoms and experiences today.
{{inline-cta-2}}
References
Abbi B., Natelson BH. “Is chronic fatigue syndrome the same illness as fibromyalgia: evaluating the ‘single syndrome’ hypothesis”. 2012. doi: https://doi.org/10.1093/qjmed/hcs156
Zambolin F. et al. “Fibromyalgia and Chronic Fatigue Syndromes: A systematic review and meta-analysis of cardiorespiratory fitness and neuromuscular function compared with healthy individuals”, 2022. doi: https://doi.org/10.1371/journal.pone.0276009
Schutzer SE et al. “Myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia are indistinguishable by their cerebrospinal fluid proteomes” 2023, doi: https://pmc.ncbi.nlm.nih.gov/articles/PMC10512920/
Jones EA. et al. “Management of fibromyalgia: An update.” 2024; doi: https://pmc.ncbi.nlm.nih.gov/articles/PMC11201510/
Castro-Marrero J, Sáez-Francàs N, Santillo D, Alegre J. “Treatment and management of chronic fatigue syndrome/myalgic encephalomyelitis: All roads lead to Rome. British Journal of Pharmacology.” 2017;174(5):345–369. doi: https://doi.org/10.1111/bph.13702
Grach SL et al. “Diagnosis and management of myalgic encephalomyelitis/chronic fatigue syndrome. Mayo Clinic Proceedings.” 2023; doi: https://doi.org/10.1016/j.mayocp.2023.07.032
Disclaimer: The Human Health app is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with your healthcare provider.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

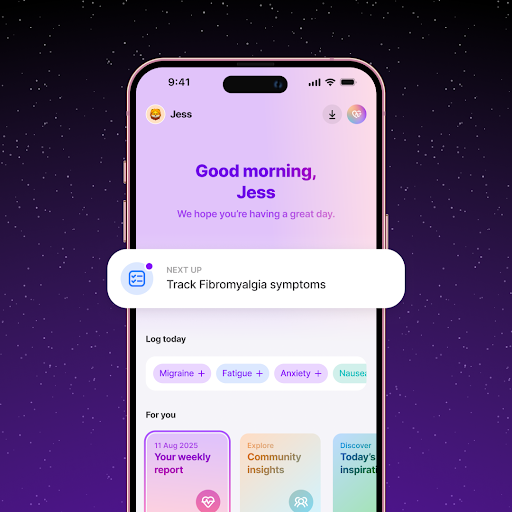
Track Fatigue and Pain with the Human Health App
Using the Human Health app log daily energy levels, pain intensity, and rest periods to understand how fibromyalgia and chronic fatigue affect your day-to-day life.
Share Detailed Insights with Your Care Team
Turn your fatigue and symptom logs into clear reports using the Human Health app - that support more informed treatment and management decisions.






Pro tip
Before your appointment, review a few weeks of symptom notes so you can describe patterns instead of single days. This can make conversations with your doctor clearer and more focused.
Pro tip
Writing down what feels hardest in daily life can help you explain impact, not just symptoms, when speaking with a healthcare provider.
Pro tip
Tracking symptoms over time may help you describe patterns more clearly during appointments.

.jpg)




.png)

