What Are the Differences Between Fibromyalgia and Migraines?
January 20, 2026

- Fibromyalgia and migraine are long-term pain conditions that can happen together and may place a heavier strain on daily life than having just one of them.
- Both conditions are linked to changes in how the brain and nervous system handle pain, which can make the body more sensitive to discomfort.
- Migraine attacks may trigger fibromyalgia pain flares in some people, with many flares happening soon after a migraine episode.
- Writing down your symptoms over time may make it easier to describe changes or patterns when you speak with your healthcare provider.
Disclaimer: This guide is for informational purposes only. It is not medical advice and should not be used to diagnose, treat, or manage any condition. Always speak with a doctor or qualified healthcare provider about any symptoms or health concerns.
Ongoing pain can be difficult to make sense of, especially when symptoms overlap.
If you’re searching for information about fibromyalgia and migraines, you’re not alone — the two often occur together and can affect the body in related ways.
This article explains how they’re connected, how they differ, and how tracking symptoms can help support clearer conversations with your doctor.
Understanding fibromyalgia and migraines
Fibromyalgia
Along-term condition linked to widespread body pain. It often includes fatigue, poor sleep, and trouble with focus or memory.
Migraine
A neurological condition marked by repeated headache attacks. These headaches can be intense and may come with nausea or sensitivity to light and sound.
Both conditions involve changes in how the nervous system processes pain signals.
What are the key symptoms of fibromyalgia and migraine
Fibromyalgia symptoms
Fibromyalgia is characterized by widespread body pain that can last for months. People may also notice deep fatigue, poor sleep, and difficulty concentrating or remembering things. Some people experience increased sensitivity to touch, light, or sound.
Migraine symptoms
Migraine involves repeated headache attacks that can last hours or days. The pain is often strong and may be felt on one side of the head. Nausea, vomiting, and sensitivity to light or sound are common during attacks.
{{pro-tip-1}}
Can fibromyalgia cause migraines?
Fibromyalgia does not directly cause migraines. The two conditions often occur together because they share changes in how the nervous system processes pain. Having one may be linked to a higher chance of experiencing the other, but only a doctor can assess this.
Possible triggers and causes
Several shared factors may explain why fibromyalgia and migraine are often seen together. These factors relate to pain sensitivity and how the body responds to stress and pain signals.
Increased pain sensitivity
Both conditions are linked to a nervous system that reacts more strongly to pain signals. This heightened sensitivity may make pain episodes more likely or more intense.
Migraine-related pain flares
In some people, migraine attacks happen shortly before fibromyalgia pain flares. This timing suggests migraines may act as a trigger for body-wide pain episodes.
Shared stress on the nervous system
Living with long-term pain, poor sleep, or emotional strain may affect how the nervous system handles signals, which could influence both migraine and fibromyalgia symptoms.
Taken together, fibromyalgia and migraine are discussed as related conditions rather than cause and effect. Their overlap appears to reflect shared pain sensitivity and nervous system stress, which is why assessment by a healthcare provider is important when symptoms occur together.
Differences and similarities between fibromyalgia and migraine
While fibromyalgia and migraine can overlap, looking at them side by side can make it easier to understand how they affect the body in different ways.
How these two conditions may affect daily life
Living with fibromyalgia and migraine may affect many parts of daily life. Ongoing body pain, fatigue, and poor sleep can make routine tasks feel harder to manage.
Migraine attacks may interrupt work, social plans, or family time because of strong head pain and sensitivity to light or sound.
When both conditions occur together, people often report a greater emotional strain, lower energy, and more difficulty keeping a regular daily routine.
{{inline-cta-1}}
Tips for managing migraines with fibromyalgia
Living with both conditions can feel overwhelming. These tips focus on awareness and communication, not treatment, and may support clearer discussions with your healthcare provider.
Tip 1: Notice symptom patterns
Pay attention to when migraines and body pain appear close together. Writing this down may help you describe possible patterns during medical appointments.
Tip 2: Track sleep and energy changes
Changes in sleep quality or daily energy often happen alongside pain. Tracking these shifts may help you explain how symptoms affect your day-to-day life.
Tip 3: Observe sensitivity to light or sound
Some people notice increased sensitivity before or during pain episodes. Recording these experiences may provide useful context for your healthcare provider.
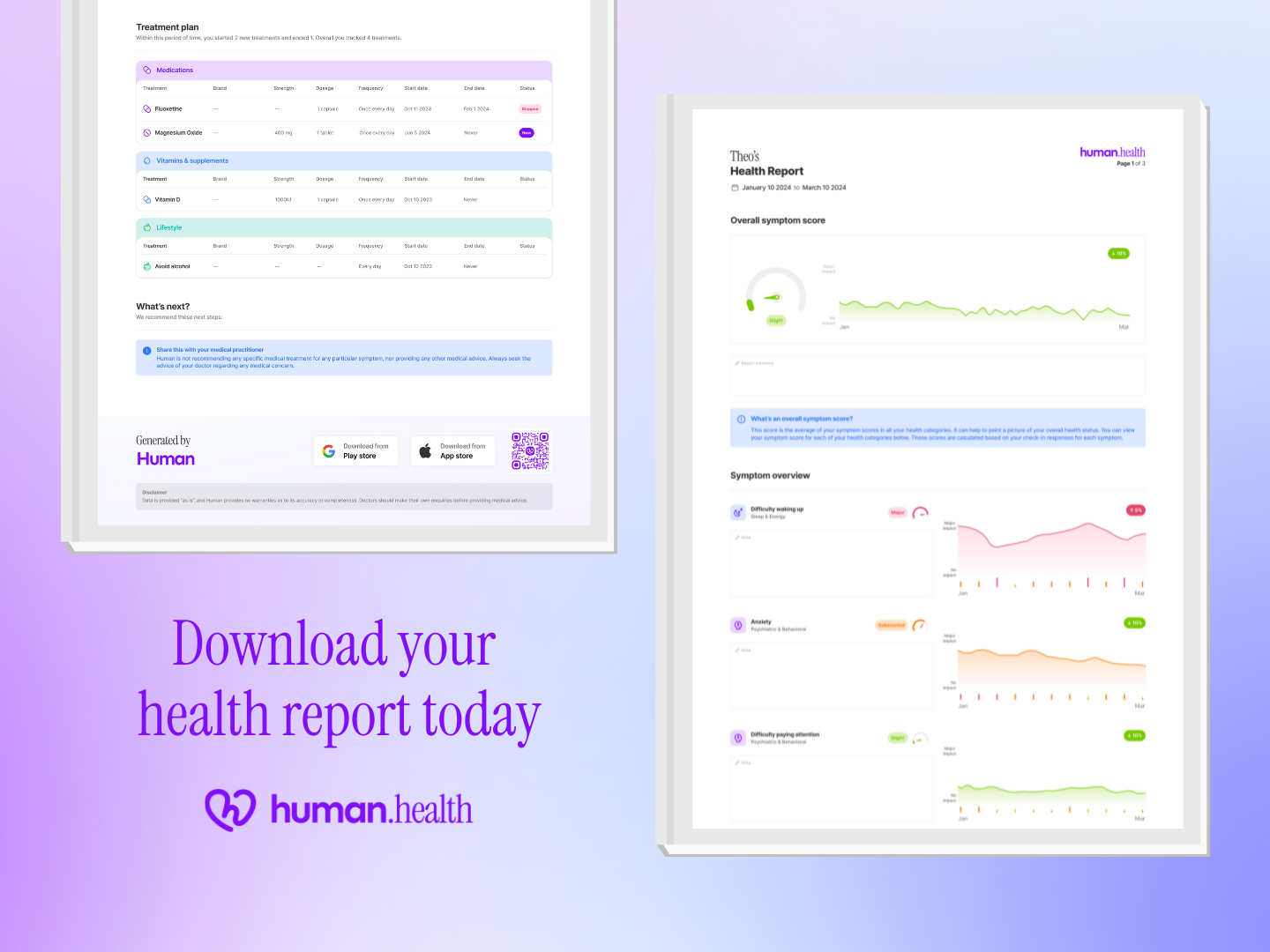
Tip 4: Use symptom tracking tools consistently
The Human Health app lets you track symptoms, daily habits, and experiences. Keeping records in one place may make it easier to share accurate information with your doctor.
Together, these approaches focus on building a clearer picture of how migraines and fibromyalgia symptoms show up over time. Having this information can support more informed conversations with a healthcare provider and help guide next steps.
When to seek medical advice
- If you have ongoing, widespread body pain that lasts for several months.
- If headaches are frequent, severe, or interfere with work, sleep, or daily activities.
- If pain is combined with long-term fatigue, poor sleep, or difficulty concentrating.
- If symptoms feel confusing, overwhelming, or are changing over time.
{{pro-tip-2}}
Track your fibromyalgia and migraine symptoms easily with the Human Health app
The Human Health app lets you track symptoms, daily habits, and experiences. You can export your information to share with your healthcare provider, helping support clearer conversations during appointments.
Start tracking your symptoms today, or read another blog to learn more about living with long-term pain.
{{inline-cta-2}}
References
Royal College of Physicians “The diagnosis of fibromyalgia syndrome. UK clinical guidelines.” 2022; https://www.rcp.ac.uk/media/udlhnt1b/the-diagnosis-of-fibromyalgia-syndrome-guidelines_1_2_0.pdf
Weatherall MK “The diagnosis and treatment of chronic migraine” 2015; https://pmc.ncbi.nlm.nih.gov/articles/PMC4416971/
Beyazal MS, Tüfekçi A et al. “The Impact of Fibromyalgia on Disability, Anxiety, Depression, Sleep Disturbance, and Quality of Life in Patients with Migraine” 2018; https://pmc.ncbi.nlm.nih.gov/articles/PMC6060661/
Calandre EP, García-Leiva JM, Ordoñez-Carrasco JL “Psychosocial Variables and Healthcare Resources in Patients with Fibromyalgia, Migraine and Comorbid Fibromyalgia and Migraine: A Cross-Sectional Study” 2022; https://pmc.ncbi.nlm.nih.gov/articles/PMC9331095/
Arnold LM, Crofford LJ “Patient Perspectives on the Impact of Fibromyalgia” 2009; https://pmc.ncbi.nlm.nih.gov/articles/PMC2564867/
Haghdoost F, Togha M “Migraine management: Non-pharmacological points for patients and health care professionals” 2022; https://pmc.ncbi.nlm.nih.gov/articles/PMC9691984/
Holroyd KA, Drew JB et al. “Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms” 2007; https://pmc.ncbi.nlm.nih.gov/articles/PMC2128721/
Giamberardino MA, Affaitati G et al. “Impact of migraine on fibromyalgia symptoms” 2016; https://pmc.ncbi.nlm.nih.gov/articles/PMC4803717/
Sastre Real M, Díaz de Terán J “OnabotulinumtoxinA Is an Effective Treatment for Chronic Migraine in Patients With Comorbid Fibromyalgia” 2020; https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2020.575130/full
Bhargava J, Goldin J “Fibromyalgia” 2025, https://www.ncbi.nlm.nih.gov/books/NBK540974/
Shapiro RE, Muenzel EJ et al. “Factors and Reasons Associated with Hesitating to Seek Care for Migraine: Results of the OVERCOME (US) Study” 2024; https://pmc.ncbi.nlm.nih.gov/articles/PMC11762058/
Disclaimer: The Human Health app is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with your healthcare provider.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

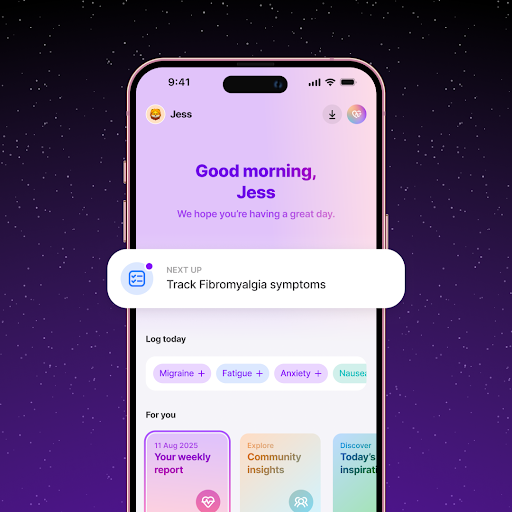
Track Migraine and Fibromyalgia Symptoms Together Using the Human Health App
With the Human Health app, you can log headache intensity, duration, and pain levels to see how migraines and fibromyalgia flare-ups overlap.
Monitor Frequency and Severity Over Time with the Human Health app
Using the Human Health app, you can track how often migraines occur and how intense they are to evaluate what management strategies are working.






Pro tip
The Human Health app lets you track symptoms, daily habits, and experiences. Writing down when pain, fatigue, or headaches appear may help you notice patterns to share with your healthcare provider.
Pro tip
Tracking symptoms over time may help you describe what you are experiencing more clearly. Notes about pain, sleep, energy, and headaches can support more focused conversations with your healthcare provider.

.jpg)




.png)

