Fibromyalgia and Arthritis: Overlaps & Management Advice
January 20, 2026

- Arthritis and fibromyalgia can feel similar, but they arise from different processes in the body.
- Arthritis involves inflammation in the joints, while fibromyalgia is linked to widespread pain and tenderness without inflammatory changes.
- Shared symptoms such as pain and stiffness can make it difficult to understand what condition is causing discomfort.
- Diagnosis relies on clinical evaluation, and overlapping symptoms may lead to delays or confusion.
- Some people choose to track their symptoms over time to notice patterns that support clearer conversations with their clinician.
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is for informational purposes only and is not a substitute for professional medical advice. Always speak with a qualified healthcare provider about any questions you have regarding your health or medical conditions.
Sorting out the difference between fibromyalgia and arthritis can feel frustrating, especially when symptoms overlap or shift from day to day.
If you’re wondering how these conditions differ, the short answer is that arthritis involves joint inflammation, while fibromyalgia causes widespread pain and tenderness without inflammatory changes.
This guide walks you through how they compare, where symptoms overlap, and what studies say about managing ongoing discomfort.
What is arthritis, and how does it differ from fibromyalgia?
Arthritis refers to inflammation in the joints, and common symptoms include joint pain, redness, heat, and swelling.
Fibromyalgia is a chronic condition that causes pain and tenderness in muscles, tendons, and joints, but does not show inflammatory changes.
Even with these distinctions, the symptoms can overlap, which may make it difficult for people to understand why they are experiencing pain in different areas.
Inflammation vs non-inflammatory pain
Arthritis is defined by joint inflammation and structural changes, while fibromyalgia does not show inflammatory changes in muscles or joints. This difference helps explain why arthritis affects joint tissues, and fibromyalgia affects pain sensitivity more broadly.
Type and location of pain
Studies comparing fibromyalgia with rheumatoid arthritis report clear differences in where pain occurs, with fibromyalgia affecting many more pain sites across the body.
Tenderness patterns
Research comparing fibromyalgia with rheumatoid arthritis found that tenderness to touch is much more common in fibromyalgia.
Pain distribution
Pain in fibromyalgia often involves the mid-lower back regions and multiple sites. Arthritis pain aligns more with affected joints, reflecting inflammation and structural change.
Despite these differences, both conditions involve pain and stiffness. These shared symptoms can make initial identification challenging, especially when people experience discomfort in several body regions.
Understanding these distinctions can make it easier to talk with a clinician about what you’re experiencing.
Could fibromyalgia possibly cause arthritis or be linked to joint damage?
Fibromyalgia can appear alongside conditions such as rheumatoid arthritis or osteoarthritis, which can make it harder to understand where certain symptoms are coming from.
The available evidence shows that fibromyalgia itself is not known to cause the joint damage seen in inflammatory arthritis. Instead, the two conditions may coexist, and their overlapping symptoms can complicate diagnosis or ongoing care.
Some studies also describe how people with inflammatory arthritis may report higher pain scores even when imaging shows little progression, which adds another layer of complexity when both conditions are present.
What symptoms might overlap between fibromyalgia and arthritis?
In a study comparing patients with fibromyalgia to patients with inflammatory conditions including rheumatoid arthritis and lupus, results show that several symptoms appear to overlap, even though the underlying conditions differ.
Both groups reported pain in multiple body regions, alongside symptoms such as fatigue, stiffness, and sleep-related difficulties.
The study also noted that people in each group described some challenges with daily activities and rated cognitive symptoms, such as memory problems.
These shared features may contribute to uncertainty when people experience symptoms across several body areas. Tracking changes in pain, fatigue, and sleep in the Human Health app can help you share a clearer picture with your clinician.
{{inline-cta-1}}
How are fibromyalgia and arthritis diagnosed?
Diagnosing these conditions can be difficult because symptoms may overlap, and pain reports do not always match what imaging or lab tests show.
Fibromyalgia
Doctors don’t have a single blood test or scan that can confirm fibromyalgia, so diagnosis is based on patterns of symptoms rather than lab results.
Diagnosis backed by data and studies
- Modern criteria from the American College of Rheumatology (ACR) focus on how many areas of your body hurt and how severe problems like fatigue, poor sleep, and thinking or memory difficulties are, instead of looking for inflammation or joint damage.
- The ACR criteria define the pain distribution in fibromyalgia as “generalized pain,” meaning pain in at least four out of five body regions that has been present for at least three months.
These criteria have shown high sensitivity and specificity in studies, meaning they can reliably tell fibromyalgia apart from other joint diseases such as rheumatoid arthritis and osteoarthritis.
Arthritis
Figuring out whether joint symptoms are caused by arthritis usually involves a few steps. Doctors don’t rely on just one test. Instead, they combine information from your symptoms, a physical exam, lab work, and imaging to understand what’s going on. This is important because there are many different types of arthritis, and they can look similar at first.
Diagnosis backed by data and studies
- Medical history: Your clinician may ask about your symptoms, when they started, how they change over time, any past injuries, infections, or illnesses, the medications you take, and whether arthritis runs in your family.
- Physical examination: A doctor will check your joints for swelling, tenderness, warmth, stiffness, and range of motion.
- Lab tests: These may include blood tests that look for signs of inflammation or specific antibodies linked to certain types of arthritis. In some cases, a doctor may remove a small amount of joint fluid to check for infection or crystals such as those seen in gout.
- Imaging tests: X-rays, ultrasound, or MRI can help show changes in bones, cartilage, or soft tissues and help confirm the type of arthritis.
Using the Human Health symptom or medication tracker can help you keep a clear record of changes over time, which can support more informed conversations during a medical evaluation.
{{inline-cta-2}}
How to manage arthritis & fibromyalgia-related joint pain
Managing joint pain linked to arthritis or fibromyalgia involves understanding your condition, following your clinician's treatment plan, and using strategies to help you stay active and monitor changes over time. Treatment varies by arthritis type, and fibromyalgia is usually approached with a combination of education, exercise, and psychological support.
1. Education
Education plays an important role in fibromyalgia care, particularly education that helps people understand how the condition can affect pain, fatigue, sleep, and daily functioning. Learning how symptoms may fluctuate and what can trigger flares can help people feel more informed and better prepared for conversations with their healthcare provider.
With arthritis, education is often more condition-specific. Different types of arthritis have different causes, diagnostic criteria, and care approaches, so understanding your specific diagnosis can help you and your clinician set more relevant goals (such as tracking joint stiffness, mobility changes, or activity tolerance over time) rather than taking a one-size-fits-all approach.
2. Exercise and physical fitness
Research shows that aerobic and flexibility exercises can help reduce fibromyalgia symptoms and support physical function. Because arthritis treatment differs by type, your clinician may guide whether exercise, mobility work, or activity adjustments are appropriate. Gentle, consistent movement can help people monitor how their joints respond over time.
{{pro-tip-1}}
3. Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) has evidence supporting its role in reducing fibromyalgia symptoms and improving coping skills. While arthritis treatments differ, people living with long-term joint pain may also benefit from therapies that support stress management and daily functioning.
The Human Health app gives you a simple way to log pain levels, exercise sessions, or therapy responses so you can notice patterns over time and share them with your clinician when needed. Try the symptom tracker to see what works for you.
When should I see a doctor?
Studies note that receiving a timely diagnosis can help reduce uncertainty and may improve satisfaction with care.
Identifying fibromyalgia early can shift the focus toward understanding symptoms and supporting quality of life. If symptoms persist, change, or cause concern, a medical evaluation can help clarify what is happening and guide next steps.
Track your overlapping symptoms & conditions
When you’re dealing with conditions like arthritis or fibromyalgia, it can feel overwhelming to keep up with pain levels, stiffness, sleep changes, and everything else your body is doing. And when symptoms shift from day to day, it’s hard to explain the full picture during a short appointment.
The Human Health app gives you a place to capture what you’re experiencing in real time, without trying to hold it all in your head.
Over days and weeks, you start to see patterns you may not have noticed before. You walk into appointments with clearer information, better questions, and a sense of confidence that you’re finally being heard and understood.
Start using the symptom tracker today to bring more clarity, calm, and control to your health journey.
References
Senthelal S, Li J, Ardeshirzadeh S, Thomas MA. Arthritis. StatPearls Publishing. 2023. https://www.ncbi.nlm.nih.gov/books/NBK518992/
Friend R, Bennett RM, Noonan C, et al. Distinguishing fibromyalgia from rheumatoid arthritis and systemic lupus erythematosus. Mayo Clinic Proceedings. 2011;86(4):413–419. doi:https://doi.org/10.4065/mcp.2010.0331
Okifuji A, Hare BD. Management of Fibromyalgia Syndrome: Review of Evidence. Pain and Therapy. 2013;2(2):87–104. doi:https://doi.org/10.1007/s40122-013-0016-9
Jahan F, Nanji K, Qidwai W, Qasim R. Fibromyalgia Syndrome: An Overview of Pathophysiology, Diagnosis and Treatment. Oman Medical Journal. 2012;27(3):192–195. doi:https://doi.org/10.5001/omj.2012.44
Bradley LA. Pathophysiology of fibromyalgia. The American Journal of Medicine. 2009;122(12 Suppl):S22–S30. doi:https://doi.org/10.1016/j.amjmed.2009.09.008
Minhas D, Bosma R, Bensen R, et al. Fibromyalgia and Centralized Pain in the Rheumatoid Arthritis Continuum: Controversies and Solutions. Rheumatology and Therapy. 2023;10(2):203–220. doi:https://doi.org/10.1007/s40744-023-00514-y
Johns Hopkins Medicine. Arthritis Diagnosis. Available at: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/arthritis-diagnosis
Ablin JN, Häuser W, Buskila D. Diagnostic criteria for fibromyalgia: Critical review and future perspectives. Journal of Clinical Medicine. 2020;9(4):1219. doi:https://doi.org/10.3390/jcm9041219
Clauw DJ. Fibromyalgia: management strategies for primary care providers. Cleveland Clinic Journal of Medicine. 2016;83(5 Suppl 1):S34–S42. doi:https://doi.org/10.3949/ccjm.83.s1.03
Disclaimer:
Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

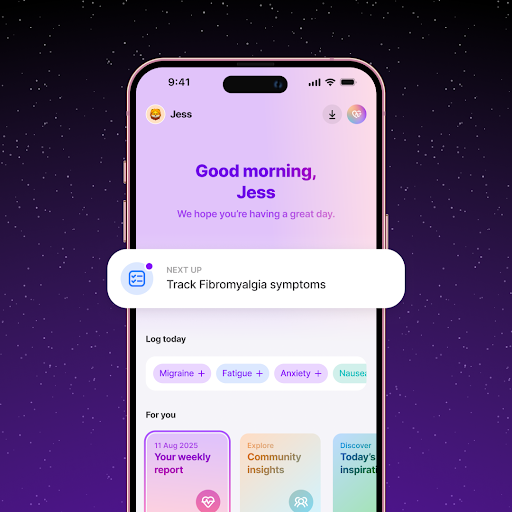
Track Joint Pain and Fibromyalgia Symptoms Together in the Human Health App
Using the Human Health app, you can log joint stiffness, swelling, and pain levels to see how arthritis and fibromyalgia symptoms overlap.
Identify Triggers that Worsen Joint Pain
With the Human Health app, you can track weather, activity levels, and stress to uncover patterns that may aggravate arthritis and fibromyalgia symptoms.






Pro tip
Make small, steady adjustments to daily routines
Gradual changes (such as easing into gentle movement, pacing activities, or setting manageable goals) can be easier to maintain than sudden shifts. This approach supports consistency and helps you build habits that fit your energy levels, treatment plan, or symptom patterns.

.jpg)




.png)

