Myalgia Vs Fibromyalgia: Differences & Management Advice
October 2, 2025

- Myalgia refers to general muscle pain, which can arise from overuse, injury, infections, or chronic health conditions. It is usually a symptom, not a disease itself.
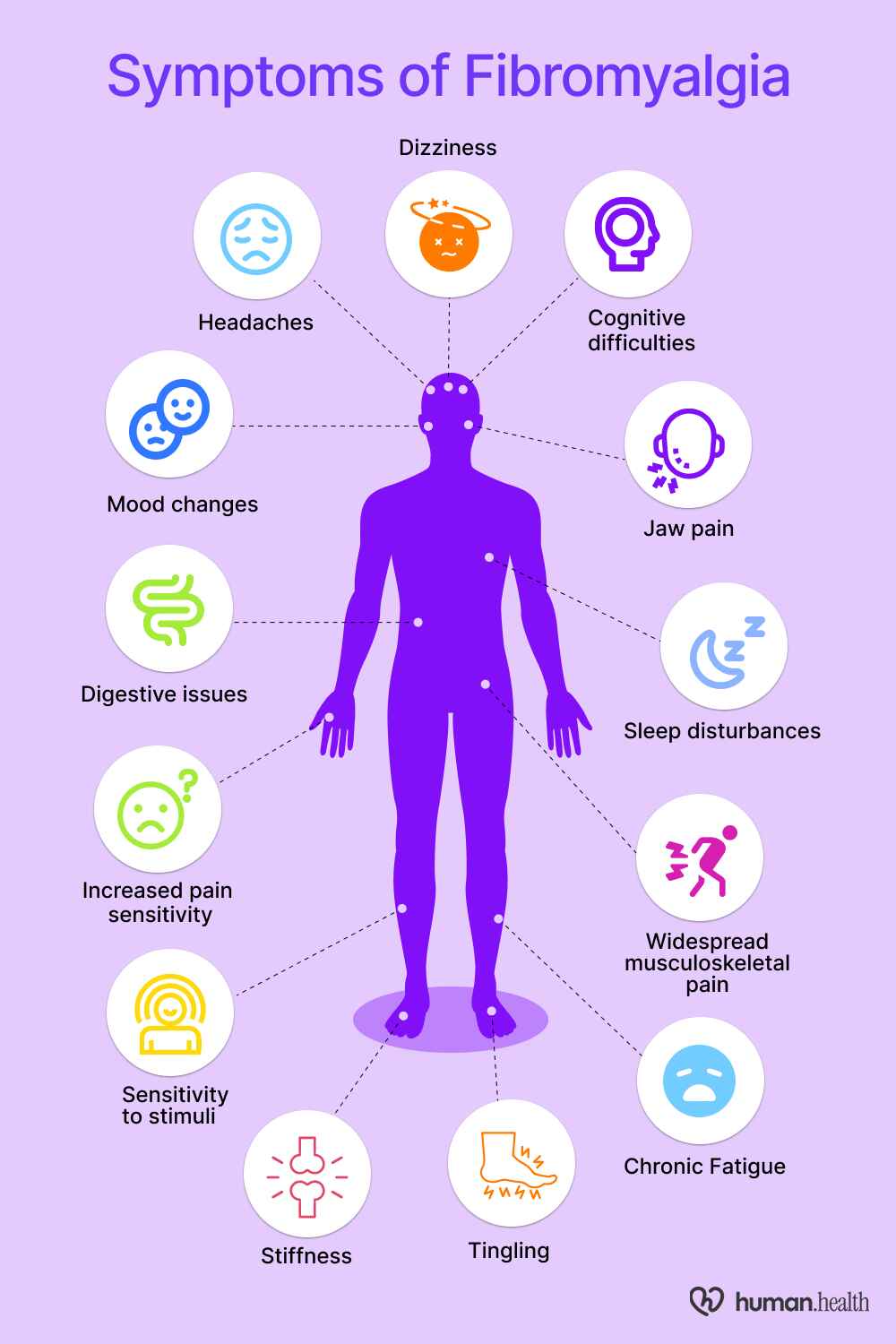
- Fibromyalgia is a chronic condition marked by widespread musculoskeletal pain, fatigue, and sleep disturbances. Unlike myalgia, it is classified as a distinct disorder with complex neurological involvement.
- The key differences lie in scope and persistence: myalgia tends to be localized and temporary, while fibromyalgia is widespread and ongoing, often accompanied by fatigue, brain fog, and mood changes.
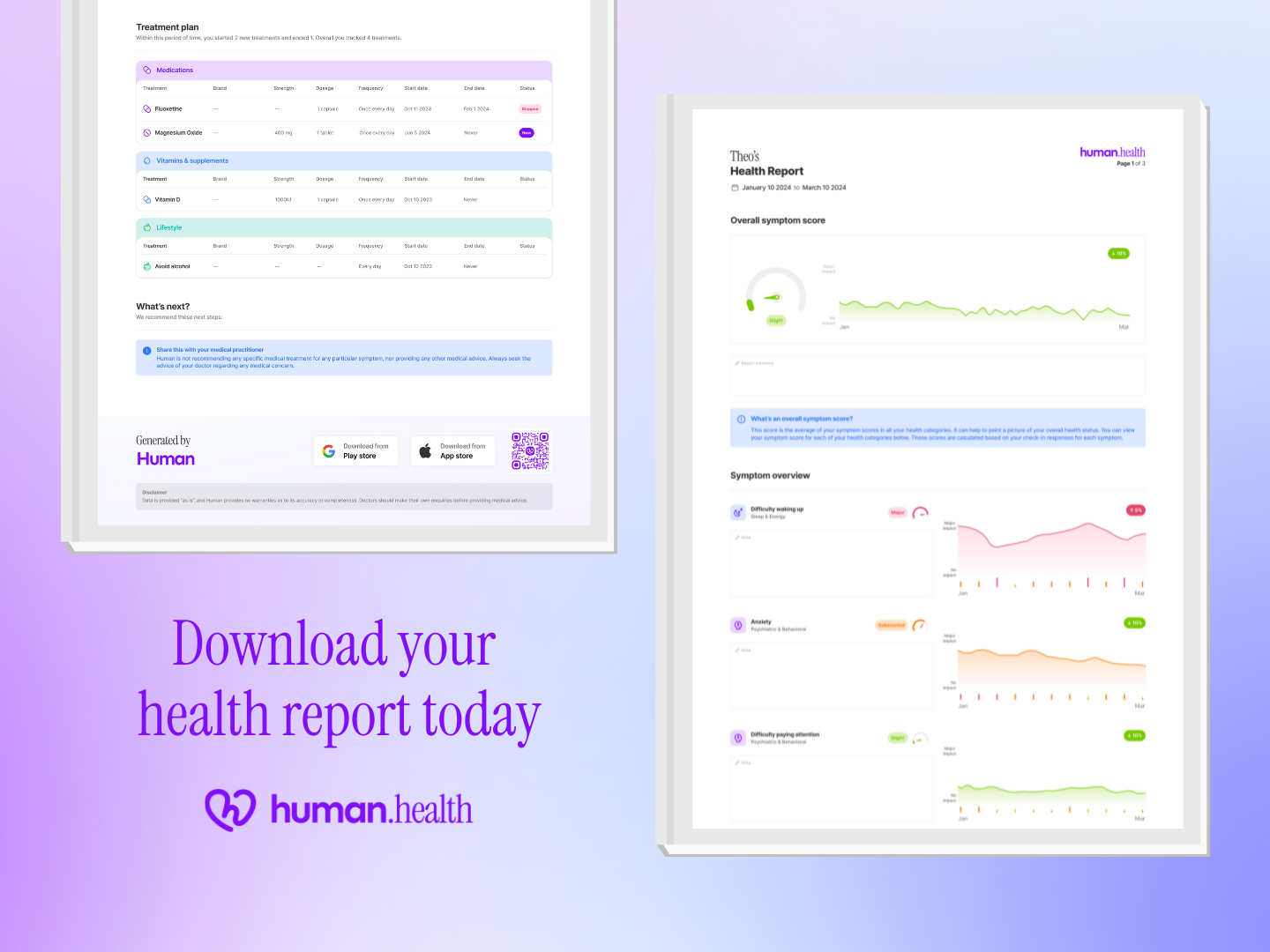
- Tracking symptoms in the Human Health app (such as pain locations, severity, fatigue, and even heart rate) can help you and your doctor identify patterns, improve communication, and manage long-term care more effectively.
Disclaimer
This article is for educational purposes only. It is not a substitute for medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider with any questions you may have about your health or a medical condition.
Living with ongoing pain can be confusing and overwhelming. If you’ve been searching for answers about myalgia vs fibromyalgia, you’re not alone. These two terms are often used interchangeably, but they describe very different experiences.
Here’s the key difference: myalgia is general muscle pain that can stem from many causes, while fibromyalgia is a chronic condition defined by widespread pain, fatigue, and other systemic symptoms.
Knowing which one applies to you matters because the right understanding can guide you toward the right care and support.
In this article, we’ll break down how these conditions connect, their symptoms and causes, and the strategies available for managing each.
The correlation between myalgia and fibromyalgia
Myalgia refers to muscle pain, while fibromyalgia is a chronic condition that often includes myalgia as one of its features. Research suggests fibromyalgia involves heightened pain processing in the central nervous system, which can make widespread musculoskeletal pain more persistent. Put simply: fibromyalgia includes myalgia, but myalgia on its own does not equal fibromyalgia.
Understanding the types of myalgia
Myalgia isn’t one-size-fits-all. Doctors often group it into different types based on what causes the pain and how long it lasts.
Acute myalgia
Acute myalgia is short-term muscle pain, often linked specifically to viral infections such as influenza. It typically resolves within days to weeks once the trigger is addressed. Multiple studies show that viral-related myalgia (as in benign acute childhood myositis) frequently occurs during influenza outbreaks (e.g., influenza B).
Chronic myalgia
Chronic myalgia is muscle pain persisting beyond a few weeks to months. Unlike acute pain, chronic muscle pain may not have a clear trigger, making diagnosis and management more complex.
Myofascial pain syndrome
Myofascial pain syndrome involves localized stiffness and pain caused by trigger points in muscles or connective tissue. It can produce referred (radiating) discomfort and limit movement. It is often mistaken for fibromyalgia, though the pain is typically confined to specific regions rather than widespread.
Knowing the type of myalgia you’re experiencing can make it easier to find the right care and to rule out conditions like fibromyalgia that bring a broader set of symptoms.
The symptoms
Myalgia can look different depending on whether it’s acute, chronic, or tied to myofascial pain. Understanding the symptom patterns is an important step toward clarity.
Acute myalgia symptoms
Acute myalgia typically presents as sudden, localized muscle soreness or stiffness. It may follow exercise, strain, or viral infections. Pain following acute muscle strain (such as in Delayed Onset Muscle Soreness) is often short-lived and resolves within a few days with conservative care, including rest. Additional symptoms can include mild swelling or tenderness in the affected muscle group.
Chronic myalgia symptoms
Chronic myalgia causes ongoing muscle pain that may shift in intensity but rarely disappears completely. It often manifests as persistent aching, stiffness, and fatigue, especially after prolonged physical activity or stress.
Myofascial pain syndrome symptoms
Myofascial pain usually presents as localized tenderness with “knots” or trigger points in the muscle. Pressing these areas may cause referred pain in nearby regions. Symptoms often include stiffness, restricted movement (motor dysfunction), and tension-type headaches when trigger points are located in neck or shoulder muscles.
These patterns highlight why it’s important to track not only the presence of pain, but also where it appears, how long it lasts, and what seems to trigger it.
{{inline-cta-1}}
Myalgia vs fibromyalgia: key differences
Myalgia and fibromyalgia are often confused, but they’re not the same. Understanding where they differ can make it easier to recognize what you might be experiencing.
Scope of pain
Myalgia usually affects a specific muscle or group of muscles, often due to strain, overuse, or infection. Fibromyalgia, in contrast, involves widespread musculoskeletal pain across multiple regions of the body, meeting the diagnostic criterion of generalized pain defined as pain in at least four of five body regions.
Duration & persistence
Myalgia is often temporary and resolves spontaneously once the triggering cause (such as muscle overuse or an acute stressor) subsides. Fibromyalgia, however, is a chronic condition that persists for months or years, requiring ongoing management and lifestyle adjustments rather than short-term recovery.
Associated symptoms
With myalgia, symptoms are typically limited to muscle discomfort, swelling, or stiffness. Fibromyalgia brings additional systemic symptoms like chronic fatigue, poor sleep, cognitive difficulties (“fibro fog”), mood changes, and even issues such as fibromyalgia weight gain. These broader effects distinguish fibromyalgia from isolated muscle pain.
Diagnosis & recognition
Myalgia is generally identified as a symptom rather than a condition on its own. Fibromyalgia, by contrast, is a recognized disorder with established diagnostic guidelines, though it remains challenging to diagnose due to overlapping symptoms with other conditions.
Keeping these distinctions in mind can help you avoid confusion and prepare more focused questions for your healthcare provider.
Myalgia vs fibromyalgia: at-a-glance comparison
Logging which muscles hurt, when pain flares occur, and how severe symptoms feel in the Human Health app can help you and your doctor determine whether you’re dealing with isolated myalgia episodes or a chronic condition like fibromyalgia.
The possible causes of the different myalgia types
The causes of muscle pain vary depending on whether it’s myalgia, fibromyalgia, or a related condition. Some triggers are temporary, while others point to deeper, ongoing issues.
Myalgia
- Muscle overuse or injury (e.g., strenuous or repetitive exercise or strain)
- Viral infections, for example, influenza
- Certain medications, such as statins
- Electrolyte imbalances, particularly low potassium
Fibromyalgia
- Changes in how the nervous system processes pain, making it feel stronger or more widespread
- A possible genetic link, since fibromyalgia often runs in families
- Physical or emotional trauma that may act as a trigger
- Coexisting health conditions such as rheumatoid arthritis or lupus
- Poor or disrupted sleep, which can increase pain sensitivity
Other types of myalgia (e.g., myofascial pain syndrome)
- Development of trigger points from muscle injury or ongoing muscle stress
- Poor posture and mechanical strain are risk factors
- Localized muscle injury can lead to hypersensitive trigger points
- Psychological stress is linked to increased muscle activity and tightness
- Myofascial pain syndrome may, in some people, progress to fibromyalgia
Knowing the possible causes won’t provide a diagnosis, but it can give you a clearer framework for tracking pain and discussing patterns with your doctor.
How doctors diagnose myalgia and fibromyalgia
Diagnosis can feel frustrating when symptoms overlap. Doctors rely on different tools and criteria to tell myalgia from fibromyalgia.
Myalgia
Myalgia is diagnosed as a symptom rather than a standalone condition. Doctors usually look for underlying causes, such as infection, medication side effects, or physical strain.
- Blood tests may reveal inflammation or electrolyte abnormalities associated with muscle disorders.
- Imaging (e.g., MRI) is used to detect or assess muscle injuries and structural issues in suspected myalgia.
- Studies show that viral infections like influenza are commonly implicated in acute myalgia / myositis.
- A detailed patient history is a foundational part of the diagnostic workup.
Fibromyalgia
Fibromyalgia is recognized as a chronic disorder requiring specific diagnostic criteria, primarily widespread pain and associated symptoms lasting at least three months.
- The 2016 American College of Rheumatology criteria emphasize widespread pain across multiple body regions, accompanied by fatigue, sleep disturbance, and cognitive symptoms.
- Blood tests and imaging are typically normal in fibromyalgia, which makes diagnosis challenging.
- Studies emphasize symptom overlap between fibromyalgia and autoimmune (and endocrine) disorders, complicating accurate diagnosis.
- Patients with fibromyalgia often experience delays of several years from symptom onset to accurate diagnosis.
Tracking pain patterns, fatigue levels, and flare frequency in the Human Health app provides valuable, time-stamped data. Using a dedicated symptom tracker like this can help your doctor differentiate between isolated myalgia episodes and chronic fibromyalgia symptoms.
Managing myalgia and fibromyalgia: Tips and advice
While there’s no single cure, people find relief by combining medical care with everyday strategies.
Gentle physical activity
Light activities such as walking, stretching, or yoga may help maintain flexibility and reduce stiffness. Studies suggest that regular low-intensity movement can improve pain perception, mood, and quality of life. Always adjust activity levels based on your comfort and provider guidance.
Stress reduction
Stress is known to exacerbate fibromyalgia and myalgia symptoms; mindfulness meditation has been shown to reduce perceived stress, improve sleep disturbance, and lessen symptom severity. Research shows that stress management is linked to improvements in perceived pain severity and quality of life in fibromyalgia.
Sleep hygiene
Poor sleep, including sleep deprivation, has been shown to worsen pain sensitivity in experimental studies. Creating a regular bedtime routine, limiting screen use before sleep, and keeping a consistent schedule may improve rest. Disrupted sleep is a core feature of fibromyalgia, and patients with non-restorative sleep report higher pain than those with good sleep.
Nutrition and hydration
Balanced nutrition and adequate hydration play supportive roles in muscle health. Studies suggest that low vitamin D levels may be linked to greater musculoskeletal pain and symptom severity in fibromyalgia.
Even small adjustments, when tracked over time, may help improve quality of life and support more productive care conversations.
Treatment approaches for myalgia and fibromyalgia and challenges
Treating myalgia and fibromyalgia often involves trial and error, with each approach offering both benefits and limitations.
#1: Medications (and limitations)
Doctors may recommend medications such as antidepressants or anticonvulsants for fibromyalgia, though their effectiveness varies widely.
#2: Physical therapy and exercise
Evidence suggests that gradual, graded exercise programmes can improve physical function in fibromyalgia and myalgia patients. However, a fibromyalgia flare up can discourage consistency, creating an ongoing management challenge.
#3: Integrative and lifestyle approaches
Mind-body techniques such as tai chi, acupuncture, or meditation show promise in reducing pain and improving quality of life, although sustained benefit often requires ongoing commitment and adaptation.
While no single method works for everyone, combining strategies and tracking progress can make long-term management more effective. For those seeking updated insights on emerging therapies, exploring new treatments for fibromyalgia can provide valuable guidance on the latest research and innovations in care.
Use the Human Health app to track myalgia and fibromyalgia symptoms (and more)
Myalgia and fibromyalgia share some overlap, but the difference between a temporary symptom and a chronic disorder is significant. Recognizing where they diverge is the first step toward finding the right support and treatment.
The Human Health app can help you take that step with confidence.
By logging pain locations, flare patterns, fatigue, and other symptoms, you create a clear record that strengthens conversations with your doctor. Over time, these insights can guide more personalized care and help you better understand your own body.
Start tracking today with the Human Health app and bring more clarity to your health journey.
Disclaimer
Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. Content here is for informational purposes only and should not replace professional medical guidance. Always consult a qualified healthcare provider about any questions you may have regarding a medical condition.
References
- National Library of Medicine: Fibromyalgia: a clinical review
- National Library of Medicine: Three cases of acute myositis in adults following influenza-like illness during the H1N1 pandemic
- Springer Nature Link: Benign acute childhood myositis: a scoping review of clinical presentation and viral etiology
- ScienceDirect: Myofascial pain – A major player in musculoskeletal pain
- American Journal of Roentgenology: Delayed-Onset Muscle Soreness: Temporal Assessment With Quantitative MRI and Shear-Wave Ultrasound Elastography
- National Library of Medicine: Anatomical and Physiological Factors Contributing to Chronic Muscle Pain
- The Journal of Headache and Pain: Myofascial trigger points in migraine and tension-type headache
- ScienceDirect: 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria
- National Library of Medicine: Myalgia and Fatigue
- National Library of Medicine: Response of Muscle and Tendon to Injury and Overuse
- National Library of Medicine: Mechanisms and assessment of statin-related muscular adverse effects
- The Lancet: Effect of statin therapy on muscle symptoms: an individual participant data meta-analysis of large-scale, randomised, double-blind trials
- ScienceDirect: Neuromuscular manifestations of electrolyte disorders
- Chapman University: Dehydration and Symptoms of Delayed-Onset Muscle Soreness in Normothermic Men
- National Library of Medicine: Enhanced central pain processing of fibromyalgia patients is maintained by muscle afferent input: a randomized, double-blind, placebo-controlled study
- National Library of Medicine: The Fibromyalgia Family Study: A Genome-Scan Linkage Study
- National Library of Medicine: Traumatic experiences, major life stressors, and self-reporting a physician-given fibromyalgia diagnosis
- Advances in Rheumatology: Fibromyalgia comorbidity in Systemic Lupus Erythematosus patients: assessing impact on quality of life
- MDPI: A Comprehensive Review of the Genetic and Epigenetic Contributions to the Development of Fibromyalgia
- National Library of Medicine: Myofascial Pain Syndrome
- National Library of Medicine: Current advances in the treatment of myofascial pain syndrome with trigger point injections: A review
- Wiley Online Library: Stress-evoked muscle activity in women with and without chronic myofascial face pain
- Mayo Clinic: Myofascial pain syndrome
- National Library of Medicine: Myopathy
- ScienceDirect: Myalgia in myositis and myopathies
- National Library of Medicine: Fibromyalgia
- National Library of Medicine: Fibromyalgia, Depression, and Autoimmune Disorders: An Interconnected Web of Inflammation
- ScienceDirect: Time to diagnosis of fibromyalgia and factors associated with delayed diagnosis in primary care
- ResearchGate: Low-Intensity Physical Exercise Improves Pain Catastrophizing and Other Psychological and Physical Aspects in Women with Fibromyalgia: A Randomized Controlled Trial
- PLOS One: Total sleep deprivation increases pain sensitivity, impairs conditioned pain modulation and facilitates temporal summation of pain in healthy participants
- National Library of Medicine: Mindfulness Meditation for Fibromyalgia: Mechanistic and Clinical Considerations
- ScienceDirect: Sleep disturbances in fibromyalgia: A meta-analysis of case-control studies
- National Library of Medicine: Vitamin D and fibromyalgia: a meta-analysis
- Springer Nature Link: Pharmacological Treatment of Fibromyalgia Syndrome: A Practice-Based Review
- ScienceDirect: Exercise as a Treatment for Fibromyalgia: A Scoping Review
- National Center for Complementary and Integrative Health: Mind and Body Practices for Fibromyalgia: What the Science Says
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Try The Human Health App Today For Free!
Gain insights into your condition, by logging in your symptoms, medications, flares, and more inside our free app!








.jpg)





.png)

