Fibromyalgia Foot Pain: Causes, Management & Relief Tips
October 23, 2025

- Fibromyalgia can affect your feet and may cause burning, tingling, stiffness, sore arches, or sensitivity that makes standing or walking more difficult.
- These sensations may be linked to nerve hypersensitivity, tender points, or overlapping conditions such as plantar fasciitis or circulation changes.
- Relief usually involves a combination of strategies: supportive shoes, gentle stretches, pacing activity, and applying heat or cold to sore areas.
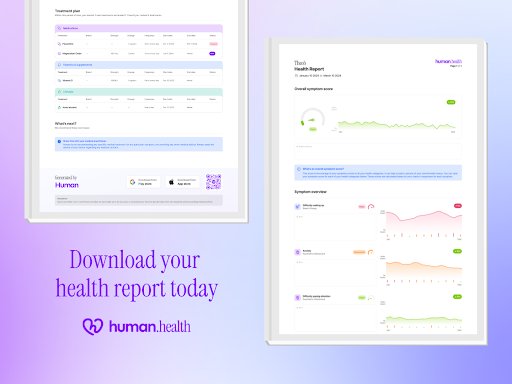
- Tracking symptoms over time with a tool like Human Health can help you log pain patterns and share clear summaries with your healthcare provider.
Disclaimer:This article is for informational purposes only and is not a substitute for medical advice, diagnosis, or treatment. Always speak with your doctor or a qualified healthcare provider about your symptoms.
If you live with fibromyalgia, foot pain may be one of the symptoms that makes daily life harder. Burning, tingling, aching, or stiff arches can turn simple moments like getting out of bed or standing in line into exhausting challenges.
This guide explains what fibromyalgia-related foot pain can feel like, how it differs from other conditions, and practical steps you can take for relief. You’ll also see how tracking symptoms with Human Health can help you notice patterns and share clearer updates with your healthcare provider.
Common symptoms of fibromyalgia foot pain
Fibromyalgia foot pain can show up in several ways. Symptoms may vary from day to day and feel worse after standing, walking, or first thing in the morning. Tracking them in the Human Health app may help you and your healthcare provider see patterns over time.
Tingling or pins-and-needles
Some people report tingling or pins-and-needles around the toes or arches. If this persists or worsens, your clinician may check for other causes.
Stiffness
Feet and ankles may feel tight or difficult to move, especially after waking or sitting still for long periods. Some people describe the stiffness easing slightly after gentle movement.
Tenderness or soreness
Sensitive spots under the heels, arches, or toes that hurt when pressed. Pain may increase after standing, walking, or wearing certain shoes.
Sensitivity when walking
Even light pressure from socks or shoes can feel uncomfortable. This sensitivity may make everyday activities (like walking short distances or standing in line) more tiring than expected.
Fibromyalgia foot symptoms may shift from burning to stiffness to soreness, sometimes all in the same day. Recognizing these patterns and noting how they change with activity, rest, or time of day may give you and your healthcare provider a clearer picture of what’s driving your discomfort.

Fibromyalgia foot pain: Is it just a standard fibro flare-up?
Research shows foot pain is common in fibromyalgia, with one study reporting it in 63% of women with the condition. This discomfort is often linked to pressure hypersensitivity and trigger points in the muscles of the feet. For some people, it becomes part of a broader flare pattern rather than a separate condition.
When should I be concerned about fibromyalgia-related foot pain?
Seek medical advice if foot pain suddenly worsens, doesn’t improve after several weeks of self-care, or is accompanied by swelling, redness, or numbness that spreads up the leg. These signs may point to another issue that requires a doctor’s assessment.
What are the other possible causes of fibromyalgia foot pain?
Research shows women with fibromyalgia report more foot pain and reduced function than healthy controls, even without major structural foot problems. This highlights how altered pain processing plays a central role in fibromyalgia-related foot pain..
Nerve dysfunction
Fibromyalgia is linked with altered pain processing and possible small fiber nerve involvement. This hypersensitivity can make the nerves in the feet respond more strongly to normal pressure or movement.
Tender points in the feet
Muscles under the arch or around the heel may contain pressure-sensitive tender points or active trigger points. These may cause soreness when standing, walking, or even pressing on specific areas.
Plantar fasciitis overlap
Some people with fibromyalgia also develop plantar fasciitis. In these cases, heel pain and stiffness may reflect both mechanical strain in the fascia and fibromyalgia’s heightened pain reactivity.
Circulation or inflammation
Low-grade systemic inflammation and changes in blood flow reported in fibromyalgia may contribute to burning or aching sensations in the feet.
{{inline-cta-1}}
Other conditions that might cause foot pain
Not all foot pain in people with fibromyalgia comes from fibromyalgia itself. It’s important to consider other conditions that may require different care.
Arthritis
Arthritis affecting foot joints can cause tenderness, swelling, stiffness, and pain, especially following rest periods.
Peripheral neuropathy
Damage to peripheral nerves can cause tingling, numbness, or burning sensations in the feet, which may feel similar to fibromyalgia pain.
You can learn more about the connection between fibromyalgia and neuropathy here.
Diabetes-related foot issues
In diabetes, prolonged high blood sugar can damage nerves and impair circulation, leading to persistent foot pain, skin changes, or non-healing sores.
Plantar fasciitis
Plantar fasciitis arises from repetitive strain or micro-tears in the plantar fascia (the ligament under the arch), and typically causes sharp heel pain with weight bearing or walking.
Circulation problems (e.g., POTS)
Blood pooling in the feet and legs due to autonomic dysfunction may cause aching, heaviness, or tingling sensations.
Connective tissue disorders (e.g., Ehlers-Danlos Syndrome)
Foot pain may also arise from joint laxity or flat feet, common in hypermobile EDS, which can overlap with but differ from fibromyalgia symptoms.
Because foot pain can come from fibromyalgia itself or other conditions, it’s worth paying attention to when it happens, what makes it worse, and how it changes over time. Sharing these details with your healthcare provider can help them pinpoint the cause and guide the most effective management plan.

How to manage fibromyalgia-related foot pain
Foot pain linked with fibromyalgia can make everyday movement (from short walks to standing in the kitchen) feel harder than it should. Small daily adjustments may help reduce discomfort and give you a bit more ease.
Choose supportive footwear
Shoes with cushioned soles, good arch support, and a wider toe box may take pressure off sensitive areas. Swapping out older, worn shoes for well-cushioned ones makes long periods of standing more bearable.
Try gentle foot stretches
Gentle movements, like flexing toes toward you or rolling the arch over a soft ball, may feel easing for some people. Stop if pain increases.
Alternate heat and cold
A warm soak may relax tight muscles, while a cold pack may settle burning or swelling after activity. Alternating the two is something you can experiment with to see which brings the most comfort.
Pace your activity
Breaking up long periods of standing or walking with short rest breaks can reduce the chance of a flare-up. Some people find setting reminders helps them step back before discomfort builds too much.
Use soft insoles or orthotics
Some people try cushioned insoles or orthotics to reduce pressure under the heel or arch. If you test them, note which designs feel better and discuss options with a clinician.
Track pain patterns
Logging when pain starts, what you were doing beforehand, and what eased it can make patterns clearer over time. This is especially useful when you want to share specifics with your healthcare provider.
The Human Health app makes this easier. You can quickly note foot pain levels, footwear changes, stretches, or flare-ups, then create a summary to bring to your next appointment.
When should you see a doctor?
You should contact your doctor if foot pain:
- Comes on suddenly or gets much worse over a short time
- Doesn’t improve after a few weeks of self-care strategies
- Is linked with swelling, redness, warmth, or visible changes in the skin or nails
- Causes numbness, tingling that spreads, or weakness in the foot or leg
Prompt attention helps rule out other conditions (such as infections, nerve issues, or circulation problems) that may need specific treatment.
Manage your condition easily with the human health app
Living with fibromyalgia foot pain can feel draining, especially when every step is unpredictable. Paying attention to patterns can make it easier to understand what triggers discomfort and what brings relief, but remembering all those details on your own is difficult.
The Human Health app gives you one place to:
- Log daily pain levels and note what was happening before a flare
- Record treatments, stretches, or footwear changes to see what helps over time
- Create clear PDF summaries to share with your healthcare provider
- Support loved ones with multi-profile tracking if you’re also a caregiver
Taking a few minutes each day to track your symptoms can help you feel more in control and give your clinician the clarity they need to guide your care and make more informed decisions about your fibromyalgia treatments.
Start today by using the Human Health app to record your foot pain patterns and build a clearer picture of your health journey.
Disclaimer: Human Health is a health tracking platform. It does not provide medical advice, diagnosis, or treatment. The information in this article is intended to support, not replace, discussions with qualified healthcare professionals.
References
- Oxford Academic: Muscle Trigger Points and Pressure Pain Sensitivity Maps of the Feet in Women with Fibromyalgia Syndrome
- National Library of Medicine: Quality of life related to foot health status in women with fibromyalgia: a case-control study
- National Library of Medicine: Fibromyalgia is associated with hypersensitivity but not with abnormal pain modulation: evidence from QST trials and spinal fMRI
- National Library of Medicine: Frequency of central sensitization and nociplastic pain in patients with plantar fasciitis
- National Library of Medicine: Is fibromyalgia associated with a unique cytokine profile? A systematic review and meta-analysis
- American College of Rheumatology: Foot and Ankle Problems in Patients With Rheumatoid Arthritis in 2019: Still an Important Issue
- Musculoskeletal Key: Neuropathic wounds: the diabetic wound
- ClinicSearch: Foot Problems in Patients with Diabetes
- National Library of Medicine: Plantar Fasciitis
- Ehlers-Danlos Support UK: Footcare in hypermobile Ehlers-Danlos syndrome
- Standing Up to POTS: POTS Subtypes
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.


Share Your Fibromyalgia Progress with Your Doctor
Use the Human Health app to generate clear, detailed symptom reports that make appointments more productive.








.jpg)





.png)

