List of Foods To Avoid With Fibromyalgia & What To Eat
October 1, 2025

- Certain foods may worsen fibromyalgia symptoms. Common triggers include highly processed foods, refined sugar, caffeine, and artificial additives.
- Diet can play a supportive role. Anti-inflammatory foods, lean proteins, fruits, vegetables, and whole grains may help reduce flare-ups and support overall health.
- Every person’s body is different. What worsens symptoms for one person may not affect another, making it essential to track and identify personal triggers.
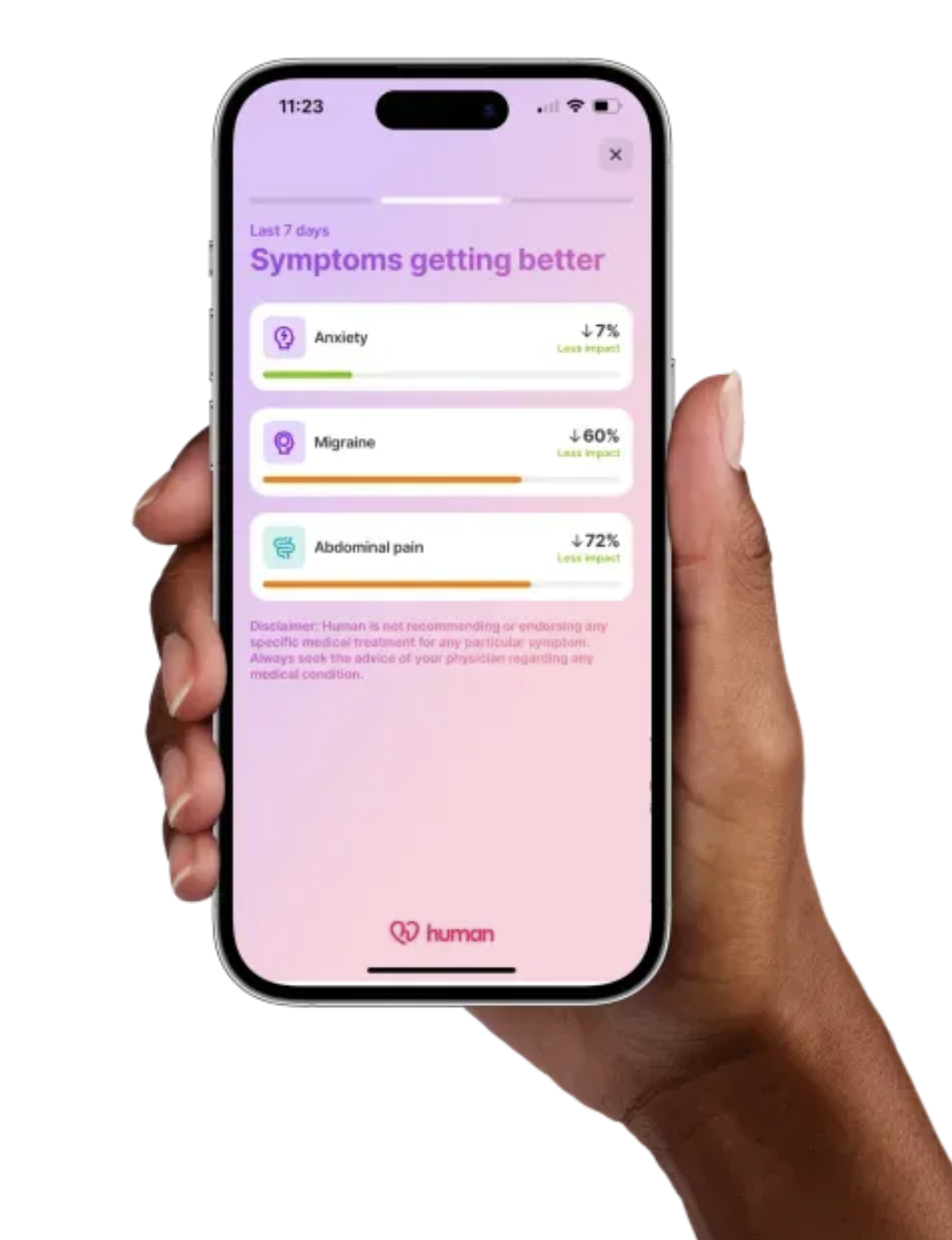
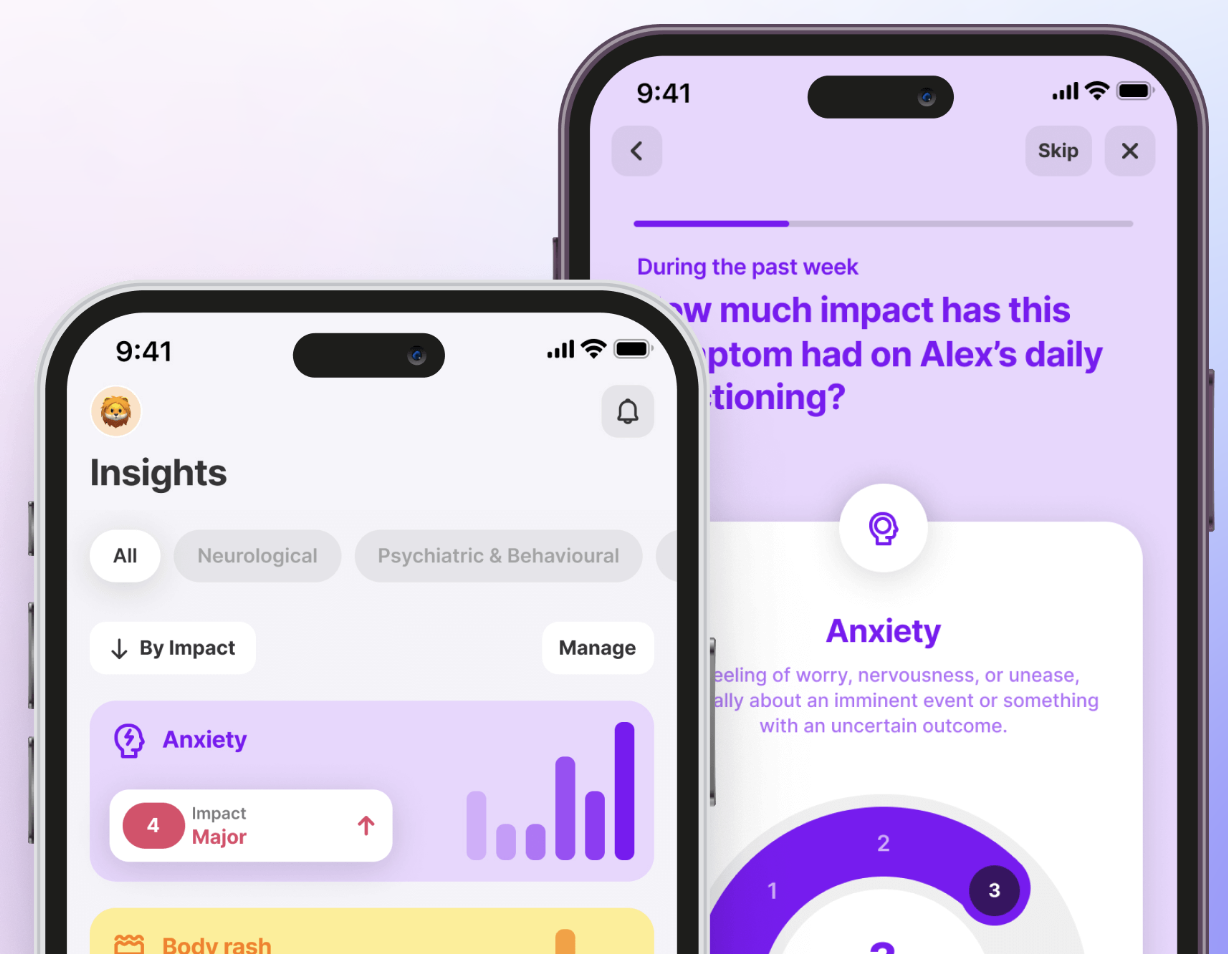
- The Human Health app can help. Use it to log meals, symptoms, and flare-ups, making it easier to uncover unique food patterns and prepare reports to share with your healthcare provider.
Disclaimer: This article is for educational purposes only and does not provide medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional before making any dietary or lifestyle changes, especially if you live with fibromyalgia or another chronic condition.
Living with fibromyalgia often feels like a constant balancing act. Pain, fatigue, and brain fog can disrupt even the simplest routines, and food choices sometimes make those symptoms better or worse.
If you have wondered which foods to avoid with fibromyalgia, and what to eat instead, this guide brings together current research and lived experiences to help you make more informed decisions.
Why diet matters for fibromyalgia
Fibromyalgia does not have a single known cause, but research shows that diet can influence how symptoms appear each day. Some foods may worsen inflammation, disrupt sleep, or increase fatigue, while others may support steadier energy, better mood, and overall quality of life. Since everyone responds differently, paying attention to your diet can be a useful way to uncover patterns and manage fibromyalgia flare-ups more effectively.
List of foods to avoid with fibromyalgia
While triggers vary by person, the following are commonly reported to increase pain, fatigue, or brain fog:
1. Refined sugar
High sugar intake can spike blood sugar levels, leading to energy crashes and increased fatigue. Some research suggests that high added sugar intake may increase inflammation and pain sensitivity. Limiting candy, pastries, and sweetened beverages may help keep energy more stable throughout the day.
2. Processed foods
Many ultra-processed foods (such as packaged meals, chips, and fast food) that are high in saturated fats, additives, and refined carbohydrates may increase inflammation and oxidative stress, which in fibromyalgia patients is linked to worse pain and fatigue.
3. Artificial sweeteners
Aspartame and other artificial sweeteners have been linked to increased pain sensitivity in some people with fibromyalgia. Evidence is mixed: a randomized crossover trial found no significant change after eliminating MSG/aspartame, while an isolated case report described symptom resolution after stopping aspartame.
4. Gluten
Evidence is limited, but one small study of 20 women with fibromyalgia found that following a gluten-free diet reduced pain and improved overall well-being. More research is needed before drawing firm conclusions.
5. Dairy products
Research on low-FODMAP and anti-inflammatory eating patterns (which reduce or eliminate multiple foods including dairy) has shown improved digestive comfort and well-being in some people with fibromyalgia. It’s unclear whether the benefits come specifically from removing dairy or from the overall diet change.
6. Caffeine
Poor sleep quality, a major challenge in fibromyalgia, is strongly linked to worse pain and fatigue, and caffeine may contribute to sleep disruption.
7. Fried foods
Fried foods high in saturated or trans fats are linked to inflammation and weight gain. In a small study of fewer than 100 participants, higher intake of these foods was associated with worse pain and fatigue in fibromyalgia.
{{pro-tip-1}}
Foods that may trigger symptoms (and why)
Recommended foods for fibromyalgia
Adding the right foods to your diet may help support energy, reduce inflammation, and improve overall well-being. Here are options to consider:
1. Fatty fish
Salmon, mackerel, and sardines are excellent sources of omega-3 fatty acids. A recent randomized controlled trial showed that high-dose omega-3 supplementation significantly reduced pain severity and symptoms in fibromyalgia patients. Try swapping fried meats or processed protein options for grilled or baked salmon.
2. Leafy greens
Spinach, kale, and Swiss chard are rich in vitamins, fiber, and minerals such as magnesium, which may support muscle relaxation and nerve function. Replace starchy side dishes with a fresh green salad or a sautéed veggie mix.
3. Berries
Blueberries, strawberries, and raspberries are rich in antioxidants, vitamin C, and fiber. These nutrients may help reduce oxidative stress, protect against cell damage, and support immune health in people with fibromyalgia. Swap sugary snacks for a bowl of mixed berries or add them to morning oatmeal.
4. Whole grains
Oats, quinoa, and brown rice are sources of complex carbohydrates and fiber; their fiber content may support digestive health, which can be a concern for people with fibromyalgia, and help maintain more stable energy over time. Replace white bread and pasta with whole-grain versions to stabilize energy levels and improve nutrient intake.
5. Nuts & seeds
Almonds, walnuts, chia seeds, and flaxseeds are nutrient-dense sources of plant-based protein, healthy fats, and minerals. Research suggests that certain nuts, especially almonds and walnuts, may help reduce markers of inflammation and oxidative stress.
A handful of nuts makes a satisfying snack, while chia pudding or almond butter on whole-grain toast can be simple swaps for sugary granola bars.
{{inline-cta-1}}
6. Legumes
Beans, lentils, and chickpeas are nutrient-dense sources of plant-based protein and fiber. While there’s no evidence that legumes directly reduce fibromyalgia symptoms, they help stabilize blood sugar, support digestive health, and provide key minerals like iron and magnesium. These benefits may indirectly ease fatigue and support steady energy, which can be valuable for people managing fibromyalgia.
7. Olive oil
Rich in monounsaturated fats and antioxidants, olive oil is a core part of the Mediterranean diet and may reduce inflammation and improve cardiovascular health in people with fibromyalgia. Replace butter or margarine with extra virgin olive oil in cooking and dressings.
8. Turmeric & ginger
Turmeric and ginger contain compounds such as curcumin and gingerol, known for their natural anti-inflammatory effects. They may help reduce stiffness, muscle pain, and inflammation, and preliminary evidence suggests potential benefit for digestive discomfort in some people. Add turmeric to soups and curries or ginger to teas and stir-fries. Swap heavy, salt-based seasonings for spice blends built around these roots.
9. Non-dairy alternatives
Almond, oat, and soy milk fortified with calcium and vitamin D can offer gentler alternatives for those sensitive to dairy and help support bone health, which can be a concern in people with fibromyalgia. Use oat milk in coffee or almond milk in smoothies instead of cow’s milk.
10. Lean proteins
Skinless chicken, turkey, and plant-based proteins like tofu deliver the amino acids your muscles need for repair without the saturated fat of red meat. Lean proteins can also help manage weight, which may reduce pain. Swap high-fat burgers for grilled chicken or marinated baked tofu as a lighter main dish.
Building your diet around these foods can give your body steady energy, but the best approach is always the one that works for you.
Restricting calories and losing weight
For some people with fibromyalgia, maintaining a healthy weight may help ease symptoms. Extra weight can place added strain on muscles and joints, which might increase pain and fatigue. Studies also suggest that obesity is linked to higher levels of inflammation, a common challenge in fibromyalgia management.
That said, weight loss should never mean drastic restriction. Instead, focusing on gradual changes (such as reducing portion sizes, swapping sugary snacks for fruits, and choosing whole grains over refined carbs) can create a gentle calorie deficit.
Always consult a healthcare provider before beginning any weight-loss plan, especially if you live with chronic conditions.
How to identify your personal food triggers
Because fibromyalgia looks different for everyone, uncovering your own food triggers is essential. These approaches can help you notice patterns with more clarity:
1. Keep a food and symptom journal
Writing down every meal, snack, and beverage (alongside how you feel afterward) can reveal patterns that aren’t obvious day to day. Over several weeks, you may notice that certain foods consistently precede flare-ups of fatigue, pain, or digestive issues. Consistency and detail are key to making this tool effective.
2. Try an elimination diet
With the help of a healthcare professional, you can temporarily remove common trigger foods such as gluten, dairy, or caffeine from your diet. After a few weeks, slowly reintroduce each item one at a time. If symptoms worsen, you’ll have stronger evidence that a specific food may be contributing to flare-ups.
3. Track timing of flare-ups
Noticing when symptoms occur is just as important as what you eat. Recording the timing of pain, brain fog, or sleep disturbances allows you to link flare-ups to recent meals or snacks. This timeline-based approach can be especially helpful when multiple foods are potential triggers.
{{pro-tip-1}}
4. Use a digital tracker
A tracker, like the Human Health app, designed for chronic conditions, can help you track symptoms and lifestyle factors, without needing to rely on memory. By logging flare-ups, noting changes in activity, or recording adjustments in routine, you’ll have a timeline that’s easy to review with your provider. Over time, this can reveal connections that might otherwise be missed.
By taking small, consistent steps, you turn meals from a source of uncertainty into an opportunity for insight.
Track progress, symptoms, and more inside the Human Health app
Diet will not cure fibromyalgia, but what you eat can influence how symptoms show up each day. By identifying which foods worsen pain or fatigue and which feel more supportive, you can create a routine that helps you feel more in control.
The Human Health app makes it simpler to log flare-ups, track changes, and share clear reports with your provider. Over time, those insights can turn trial and error into a more confident, collaborative approach to care.
Disclaimer: This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions regarding your condition or before making changes to your diet, medications, or lifestyle.
References
- MDPI: Dietary Effects on Pain Symptoms in Patients with Fibromyalgia Syndrome: Systematic Review and Future Directions
- MDPI: Nutrition and Chronobiology as Key Components of Multidisciplinary Therapeutic Interventions for Fibromyalgia and Associated Chronic Fatigue Syndrome: A Narrative and Critical Review
- Preprints: Evaluation of Ultra-Processed Food Intake and Inflammatory Dietary Pattern in Adults With Fibromyalgia Syndrome. A Case-Control Study
- National Library of Medicine: Monosodium glutamate and aspartame in perceived pain in fibromyalgia
- ResearchGate: Aspartame-induced fibromyalgia, an unusual but curable cause of chronic pain
- National Library of Medicine: Efficacy of a gluten-free diet in reducing the widespread pain index and symptom severity scale in patients affected by fibromyalgia
- Frontiers in Nutrition: An anti-inflammatory and low fermentable oligo, di, and monosaccharides and polyols diet improved patient reported outcomes in fibromyalgia: A randomized controlled trial
- National Library of Medicine: The association between pain and sleep in fibromyalgia
- BMC: Association between alcohol consumption and symptom severity and quality of life in patients with fibromyalgia
- National Library of Medicine: Proinflammatory diet is associated with higher pain, disease severity and biochemical parameters associated with inflammation in fibromyalgia
- American Fibromyalgia Syndrome Association (AFSA): Diet & Nutrition for Fibromyalgia
- National Library of Medicine: Neuronutritional Approach to Fibromyalgia Management: A Narrative Review
- National Library of Medicine: High-dose Omega-3 Alters Serum Magnesium and Calcium Levels and Affects Fibromyalgia Symptoms: A Randomized, Double-blind, Placebo-Control Study
- MDPI: Antioxidant Treatments for Fibromyalgia
- National Library of Medicine: Diet and Lifestyle Modifications for Fibromyalgia
- National Library of Medicine: Effect of Nuts on Markers of Inflammation and Oxidative Stress: A Narrative Review
- MDPI: Effects of Olive Oil Consumption on Cardiovascular Risk Factors in Patients with Fibromyalgia
- ScienceDirect: Legume Consumption and Cardiometabolic Health
- National Library of Medicine: Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials
- Journal Bone Fragility: Plant-based diets and bone health
- PAIN Reports: Fibromyalgia in women: association of inflammatory plasma proteins, muscle blood flow, and metabolism with body mass index and pain characteristics
- National Library of Medicine: Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Journal & Track Your Condition Inside Our App
The Human Health app allows you to log symptoms, medications, receive reminders and more, all in one place!







Pro tip
Focus on consistency, not perfection. Even small, steady changes in how you eat can reveal patterns that wild swings in diet might hide.
Pro tip
Log flare-ups as soon as they happen. Capturing symptoms in real time makes the link between food and fibromyalgia symptoms far clearer than trying to recall them later.

.jpg)





.png)

